Head and neck cancers with synchronous primary cancers in Ireland
Purpose/Objective
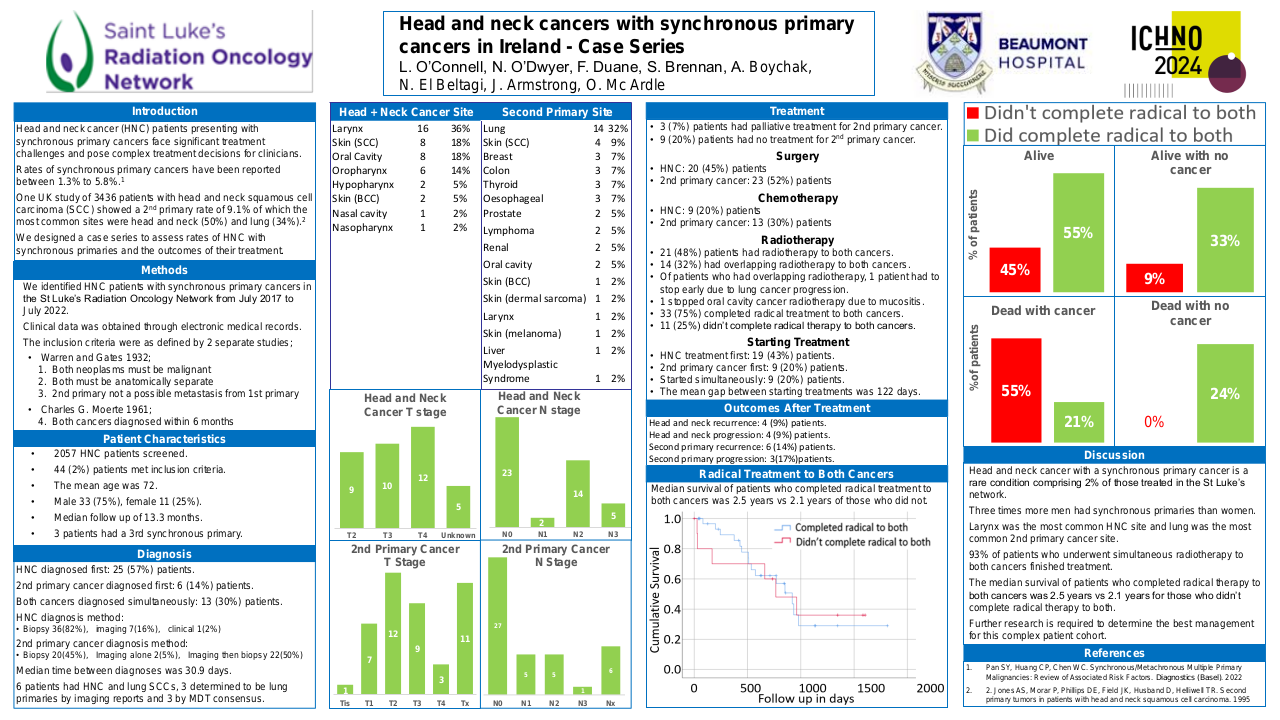
Head and neck cancer (HNC) patients presenting with synchronous primary cancers face significant treatment challenges and pose complex treatment decisions for clinicians. Rates of synchronous primary cancers have been reported between 1.3% to 5.8%.1 One study in the UK of 3436 patients with head and neck squamous cell carcinoma (SCC) identified a second primary rate of 9.1% of which the most common sites were head and neck (50%) and lung (34%).2 We designed a case series to assess rates of HNC with synchronous primary cancers and the outcomes of their treatment.
Material/Methods
We identified HNC patients with synchronous primary cancers in the St Luke’s Radiation Oncology Network from July 2017 to July 2022. Clinical data was obtained through review of patients electronic medical records. The inclusion criteria we used were as defined by two separate studies; Warren and Gates 1932; both neoplasms must be malignant, both must be anatomically separate, second primary must not be a possible metastasis from the first primary and Charles G. Moerte 1961; both cancers diagnosed within 6 months.
Results
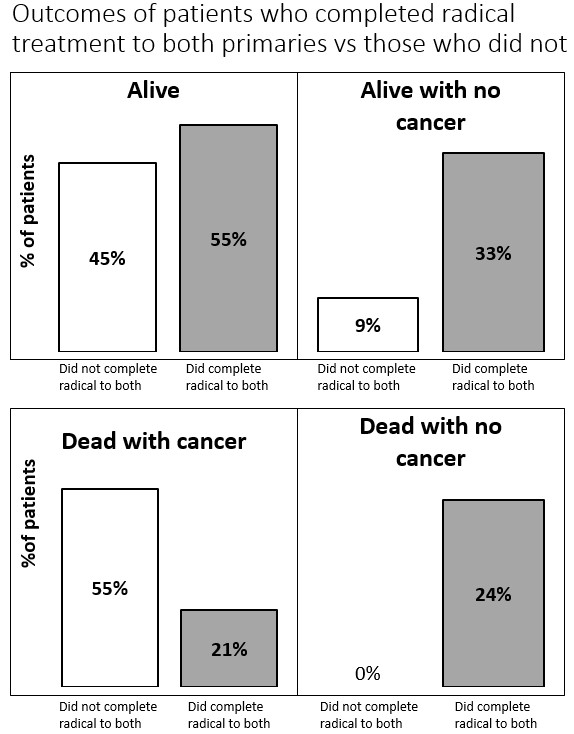
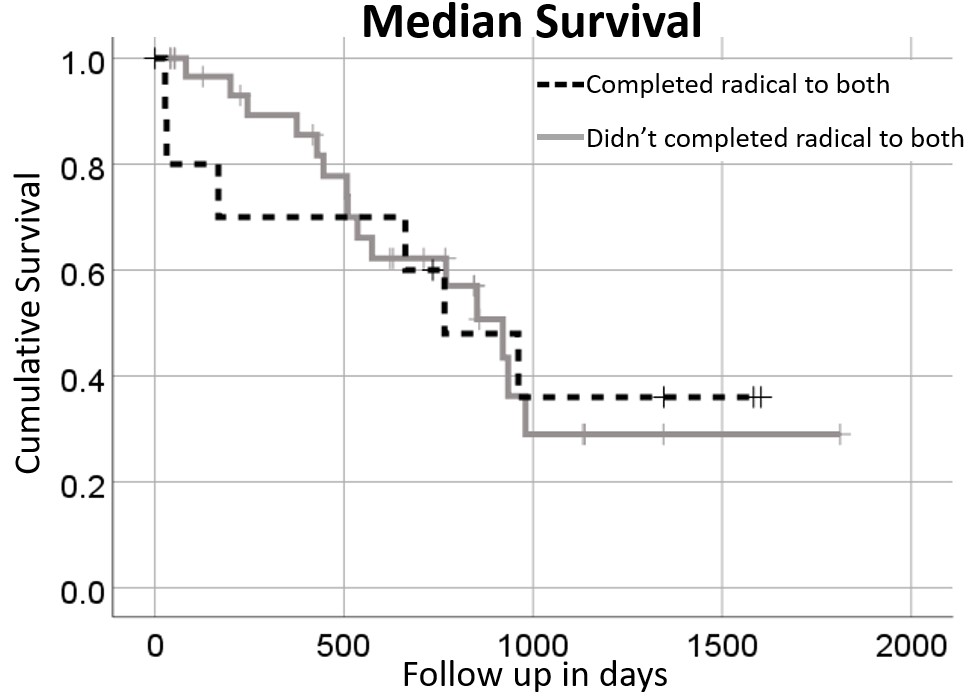
We screened 2057 HNC patients who underwent radiotherapy. Forty-four (2%) patients met the inclusion criteria. The mean age was seventy-two. Seventy-five percent of the patients were male and 25% were female. The median follow up was 13.3 months. The most common HNC sites were laryngeal with 36% of patients, skin and oral cavity with 18% of patients each and oropharynx with 14% of patients. For TNM staging of the HNC, none were T1, 20% were T2, 23% were T3, 28% were T4 and 11% were unknown. For N staging, 52% were N0, 4% were N1, 32% were N2 and 11% were N3. The most common second primary cancer sites were lung with 32% of patients, skin with 9% of patients followed by breast, colon, thyroid and oesophageal all with 7% of patients each. HNC was diagnosed first in 57% of patients, the second primary cancer was diagnosed first in 14% of patients and the cancers were diagnosed simultaneously in 30% of patients. Six patients had squamous cell carcinoma HNC and lung cancer, the lung cancers were deemed separate primaries via multidisciplinary team consensus. The patients’ treatments were as follows; 45% had surgery for their HNC, 52% had surgery for their second primary cancer, 20% had chemotherapy for their HNC, 30% had chemotherapy for their second primary cancer, all patients had radiotherapy to their HNC and 48% of patients had radiotherapy to both cancers. Of patients who had simultaneous radiotherapy one patient had to stop early due to lung cancer progression and one patient stopped oral cavity cancer radiotherapy early due to mucositis. Three (7%) patients had palliative treatment for their second primary cancer. One patient died due to treatment, five days after pneumonectomy due to trachea-oesophageal fistula and subsequent aspiration. There were no other deaths attributed to treatment but the causes of death were unknown for two patients. Seventy-five percent of patients managed to complete radical treatment to both cancers. The median survival of patients who completed radical treatment to both cancers 2.5 years versus 2.1 years among patients who did not. Outcomes at the end of follow up for patients who completed radical treatment to both cancers versus those who did not are as follows; alive (55% versus 45%), alive with no cancer (33% versus 9%), dead with cancer (21% versus 55%) and dead with no cancer (24% versus 0%).
Conclusion
Head and neck cancer with a synchronous primary cancer is a rare condition comprising 2% of those treated in the St Luke’s network. Three times more men had synchronous primary cancers than women. Larynx was the most common HNC site and lung was the most common second primary cancer site. The majority of patients who underwent simultaneous radiotherapy to both cancers finished treatment. The median survival of patients who completed radical therapy to both cancers was 2.5 years versus 2.1 years for those who did not complete radical therapy to both. There was a higher percentage of patients alive and without cancer at the end of follow up among patients who completed radical treatment to both primary cancers than those who did not. Further research is required to determine the best management for this complex patient cohort.
1. Pan SY, Huang CP, Chen WC. Synchronous/Metachronous Multiple Primary Malignancies: Review of Associated Risk Factors. Diagnostics (Basel). 20222. Jones AS, Morar P, Phillips DE, Field JK, Husband D, Helliwell TR. Second primary tumors in patients with head and neck squamous cell carcinoma. 1995