Adjuvant radiation therapy for anaplastic thyroid cancer: single center experience of 12 patients with advanced and not completely resected disease: toxicity and treatment complications
Purpose/Objective
To evaluate acute toxicity and treatment complications in patients receiving adjuvant radiation therapy for advanced anaplastic thyroid cancer in cohort of patients who have not underwent complete R0 surgery. Find correlations between incompletment of radiation therapy, doses to organs at risk and completeness of surgical treatment.
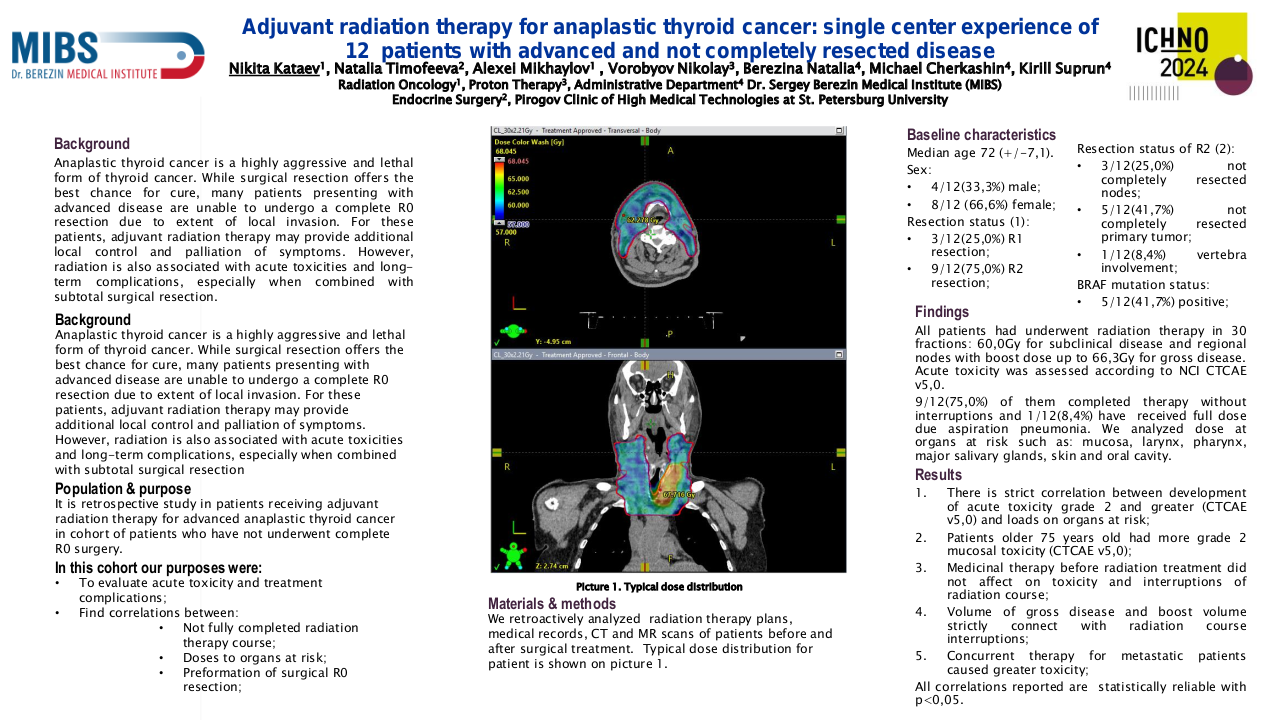
Material/Methods
We retroactively analysed plans, medical records, CT and MR scans of patients before and after surgical treatment. In our analysis were included total 12 patients between 2021 and 2023. Median age of patients was 72 (+/-7,1).
4/12(33,3%) were male, other 8/12 (66,6%) were female.
3(25,0%) patients had R1 resection and 9(75,0%) had R2 resection.
3(25,0%) had not completely respected nodes. 5(41,7%) had part of primary tumor not removed. And 1(8,4%) had vertebra involved which wasn’t completely respected.
9(75,0%) had involved regional nodes by pathology report. 4(33,3%) were metastatic patients.
All of them were tested for BRAF mutation and 5(41,7%) were positive for this mutation.
All patients had underwent radiation therapy in 30 fractions: 60,0Gy for subclinical disease and regional nodes with boost dose up to 66,3Gy for gross disease. Acute toxicity toxicity was assessed according to NCI CTCAE v5,0.
9/12(75,0%) of them completed therapy without interruptions and one(8,4%) have received full dose due aspiration pneumonia. We analysed dose at organs at risk such as: mucosa, larynx, pharynx, major salivary glands, skin and oral cavity. We searched correlation between surgery treatment attributes, volume and type of gross disease, loads on organs at risk.
Results
1 We found strict correlation between development of acute toxicity grade 2 and greater (CTCAE v5,0) and loads on organs at risk.
2 We also found that patients older 75 years old had more grade 2 mucosal toxicity (CTCAE v5,0).
3 Medicinal therapy before radiation treatment did not affect on toxicity and interruptions of radiation course.
4 We also found that volume of gross disease and boost volume strictly connect with radiation course interruptions.
5 Concurrent therapy for metastatic patients caused greater toxicity.
All correlations reported are statistically reliable with p<0,05.
Conclusion
For those patients volume of gross disease after surgery can affect on completeness of radiation treatment. We also found that age, concurrent therapy and doses on organs at risk can affect on treatment tolerance and toxicity.