Lobectomy vs total thyroidectomy for papillary thyroid carcinoma with lymph node metastasis
Purpose/Objective
Although the guidelines recommend total thyroidectomy (TT) and subsequent radioactive iodine ablation as the management options for patients with papillary thyroid carcinoma (PTC) and lymph node metastasis, the direct evidence for this management is lacking [1]. Currently, there are few studies comparing unilateral lobectomy (uLT) and TT for patients with unilateral PTC and ipsilateral cervical lymph node metastasis (IC-LNM) [2, 3]. The present study was carried out to compare the prognosis of patients with unilateral PTC and IC-LNM treated with uLT vs TT so as to find out which surgery was optimal for these patients without other clinical risk features.
Material/Methods
Thyroid cancer patients at Zhejiang Cancer Hospital between February 2012 and January 2022 were retrospectively reviewed. Patients with unilateral PTC and IC-LNM who underwent uLT or TT for the primary tumor and simultaneous ipsilateral cervical lymph node dissection were included in this study. Patients with any of the following features were excluded: bilateral lobe tumors; tumor size ≥ 4 cm; extensive extrathyroidal invasion; with contralateral cervical lymph node metastasis; distant metastasis; non-primary surgery. Additionally, a propensity score matching (PSM) was performed on patients treated with u-LT or TT. Recurrence-free survival (RFS), overall survival (OS), hospitalization costs, postoperative complications, and other clinical characteristics were compared between the two groups.
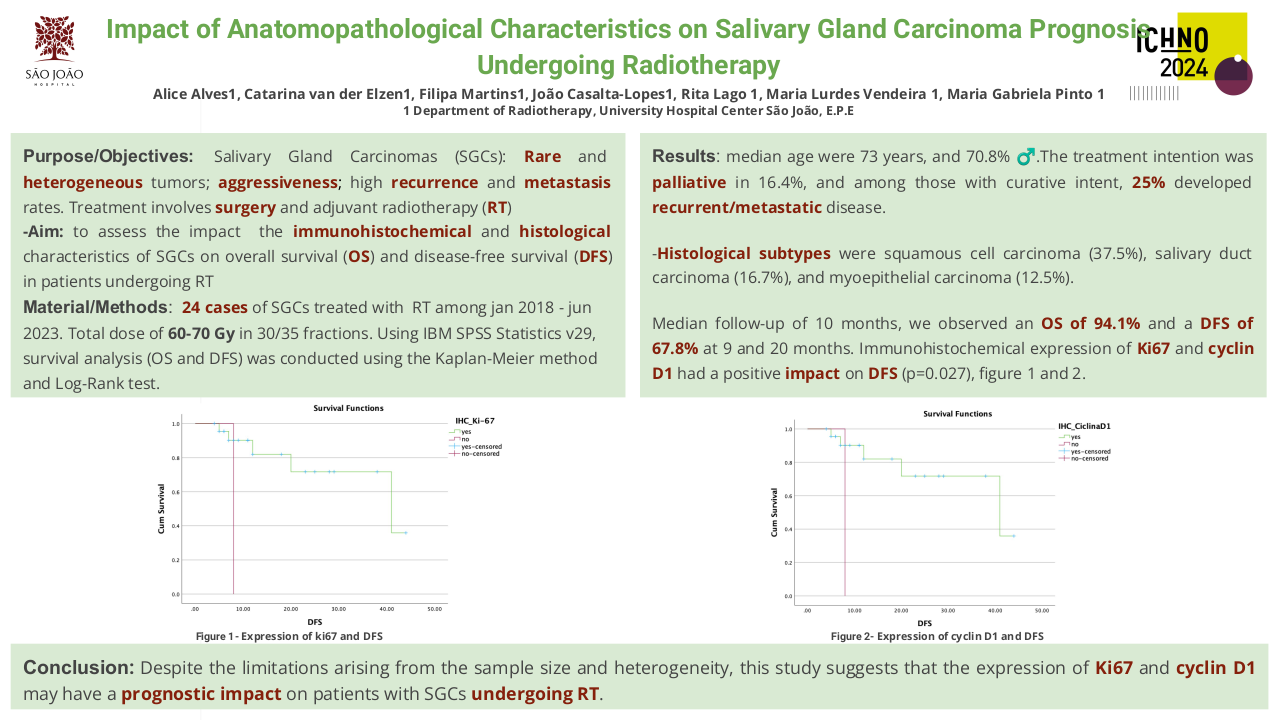
Results
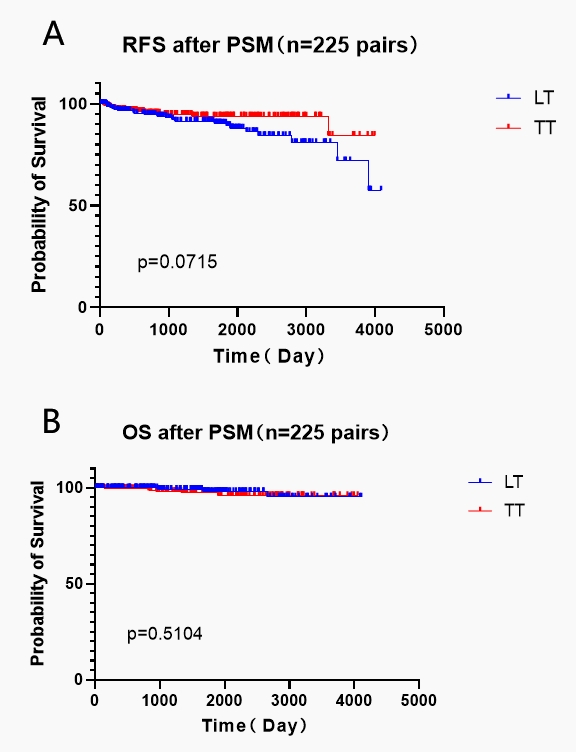
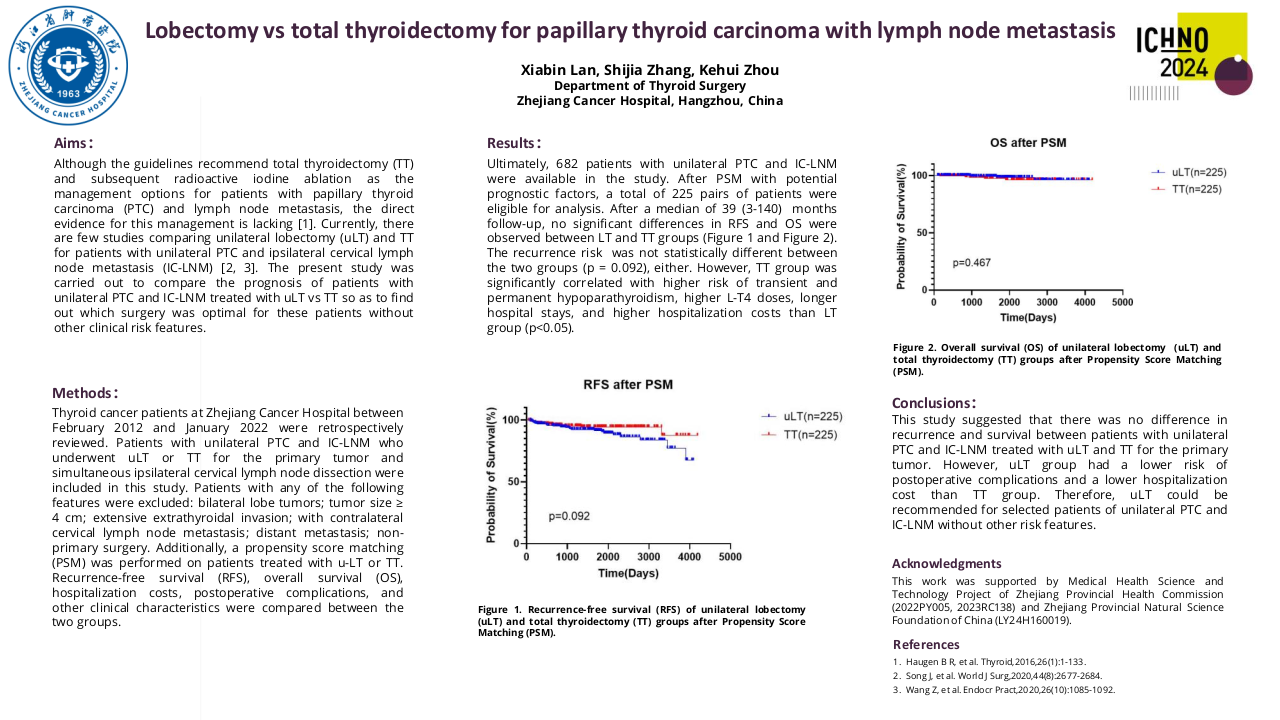
Ultimately, 682 patients with unilateral PTC and IC-LNM were available in the study. Among the 682 patients, 443 (65.0%) patients were treated with uLT and 239 (35.0%) patients were treated with TT. After PSM with potential prognostic factors (such as gender, age, primary tumor size, multifocality, extrathyroidal invasion, and T stage), a total of 225 pairs of patients were eligible for analysis. After a median of 35 months (range: 16 - 4160 days) follow-up, 22 (10.1%) and 12 (5.4%) patients experienced recurrences in the uLT group and TT group, respectively. The recurrence risk in the TT group was not statistically different from that in the uLT group (adjusted hazard ratio = 0.540; 95% CI, 0.265-1.097; p = 0.088). No significant differences in RFS and OS were observed between uLT and TT groups (Figure 1). However, TT group was significantly related with higher risk of transient and permanent hypoparathyroidism (p< 0.01), higher L-T4 doses (p< 0.001), longer hospital stays (p< 0.01), and higher hospitalization costs (p< 0.001) than uLT group.
Figure 1. Recurrence-free survival (RFS, A) and overall survival (OS, B) of lobectomy (LT) and total thyroidectomy (TT) groups after propensity score matching (PSM)
Conclusion
This study suggested that there was no difference in recurrence and survival between patients with unilateral PTC and IC-LNM treated with uLT and TT for the primary tumor. However, uLT group had a lower risk of postoperative complications and a lower hospitalization cost than TT group. Therefore, uLT could be recommended for selected patients of unilateral PTC and IC-LNM without other risk features.
1. Haugen B R, Alexander E K, Bible K C, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid,2016,26(1):1-133.2. Song J, Qiu W, Yan T, et al. Comparison of Lobectomy and Total Thyroidectomy in Unilateral Papillary Thyroid Microcarcinoma Patients with Ipsilateral Lateral Lymph Node Metastasis Without Gross Extrathyroidal Extension. World J Surg,2020,44(8):2677-2684.3. Wang Z, Xiang J, Gui Z, et al. Unilateral Tnm T1 And T2 Papillary Thyroid Carcinoma With Lateral Cervical Lymph Node Metastasis: Total Thyroidectomy or Lobectomy?. Endocr Pract,2020,26(10):1085-1092.