Landscape of esophageal cancer in Kenya: Experience from Garissa Regional Cancer Center
Purpose/Objective
In Kenya, cancer is the second leading cause of non-communicable disease deaths, and the trend of cancer deaths is projected to increase as per the 2018 GLOBOCAN report showing 47,887 new cases annually with a mortality of 32,987. Common cancers in men in Kenya are esophageal cancers (EC), prostate, colon, and rectum cancers. In contrast, breast, cervical, and EC are the leading cancers in women. However, EC is the most diagnosed cancer in both males and females and the leading cancer-related mortality in Kenya.
Published studies regarding the epidemiological factors that may or may not drive the high incidence of EC in Kenya include poor diet and nutritional insufficiencies with high intake of red meat, use of alcohol and tobacco, environmental carcinogenic exposure, intake of hot beverages, and genetic susceptibility citing a remarkable positive close family history of esophageal cancers.
Despite the availability of radiation and chemotherapy services at the Garissa Regional Cancer Center (GRCC), there is limited data about the clinicopathologic features and treatment outcomes of EC in this region. Therefore, this is the first study to look at the epidemiological patterns of EC in the northern Kenya region.
Material/Methods
This was a retrospective study involving patients’ file review of confirmed EC cases diagnosed or treated at the GRCC, a regional referral cancer center between 2019 and 2023. Data collected on each patient’s chart included age, sex, risk factors, family history, histological type, stage at diagnosis, treatment type, and survival outcomes. For patients who were no longer in contact with the staff through clinic visits, the patients or their next of kin were contacted through phone calls for patients’ survival status. Data were collected and stored using the STATA software.
Results
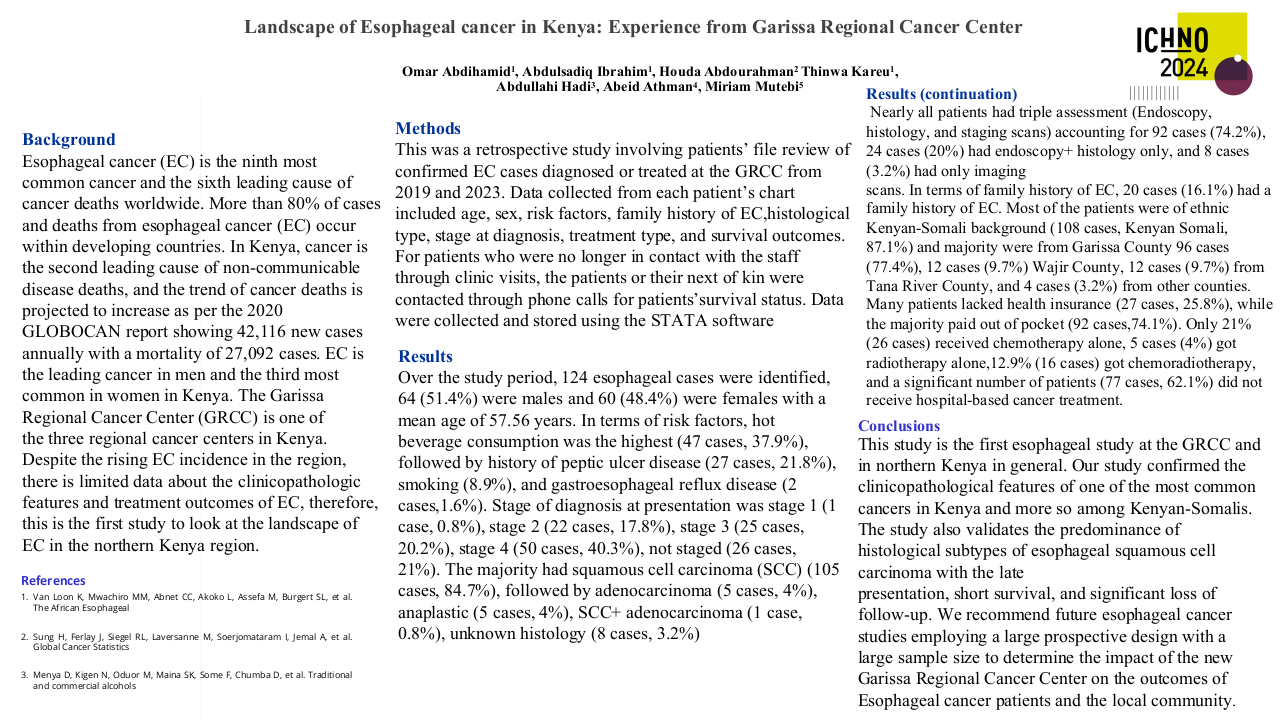
124 esophageal cases were identified, 64 (48%) were males and 60 (52%) were females with a mean age of 57.56 years. In terms of risk factors, hot beverage consumption was the highest (47 cases, 57%), followed by history of peptic ulcer disease (27 cases, 33.5%), smoking (8.9%), gastroesophageal reflux disease (2 cases, 1.6%), unknown (8.7%), and 37% of the patients were lost to follow up with no identifiable risk factors.
Stage of diagnosis at presentation was stage 1 (1 case, 0.8%), stage 2 (22 cases, 17.8%), stage 3 (25 cases, 20.2%), stage 4 (50 cases, 40.3%), not staged (26 cases, 21%). The majority had squamous cell carcinoma (105 cases, 84.7%), followed by adenocarcinoma (5 cases, 4%), anaplastic (5 cases, 4%), SCC+ adenocarcinoma (1 case, 0.8%), unknown histology (4 cases, 3.2%).
In terms of diagnostic modality, 92 cases (74.2%) had triple modality assessment (Endoscopy, histology, and staging scans), 4 cases (3.2%) had only imaging scans, and 24 cases (20%) had endoscopy+ histology only.
20 cases (16.1%) had a family history of cancer (irrespective of sub-type). Most of the patients were of ethnic Kenyan-Somali background (108 cases, Somali, 87.1%), and other tribes (7 cases, 0.6%). 96 cases (77.4%) were from Garissa County, 12 cases (9.8%) were from Wajir county, 12 cases (12.8%) from Tana River County, and 4 cases (3.2%) from other counties. Most patients paid cash for their treatment (92 cases,77%) while only (27 cases, 23%) paid through the National Hospital Insurance Fund (NHIF).
Conclusion
This study is the first esophageal study in northern Kenya and confirmed the clinicopathological features of one of the most common cancers in Kenya and more so among Kenyan-Somalis. The study also validates the predominance of histological subtypes of esophageal squamous cell carcinoma with the late presentation, short survival, and significant loss of follow-up.
Our data demonstrates the need for the county government of Garissa in collaboration with the National Cancer Control Program to prioritize EC on the national health agenda, including promoting preventative strategies, cost-effective early screening, early detection, and timely treatment and designing interventions to improve treatment adherence such as using appointment reminders via mobile phones, setting up an up-to-date cancer registry, and enhancing referral pathways. We recommend future esophageal cancer studies employing a large prospective design with a large sample size to determine the impact of the new GRCC on the outcomes of Esophageal cancer patients and the local community.