nasopharyngeal cancer in children: understanding, diagnosing and treating
Purpose/Objective
Nasopharyngeal cancer presents clinical, therap,eutic and progressive particularities; it is a chemo-
and radiosensitive disease, its management is complex due to the lack of specific trials for children.
Primary aim was evaluating the role of radiotherapy in the management of nasopharyngeal cancer in
children .And describing the epidemiological, clinical assecondary aims .
Material/Methods
A retrospective analysis of patients aged under 15 years, and treated for nasopharyngeal cancer
between January 2017 and december 2020 in the radiotherapy department of the National
Institute of Oncology in Morocco ; data were collected from medical records.
Results
Twenty patients were collected, the median age was 13 years, the tumors were classified as stage III
in 9 cases (45%) and stage IVA in 11 cases (55%). One patient (5%) was metastatic at the time of
diagnosis, 13 patients (65%) received induction chemotherapy with TPF (docetaxel, cisplatin, 5FU), 2
(10%) with ECF (epirubicin, cisplatin,5FU).
After a median follow-up of 24 months, 4 patients (20%) presented with a metastatic relapse, and
one patient (5%) presented with local regional or distant . Overall survival at 2 years was is 90%.
In subgroup analysis, a number of courses greater than 4 or greater than 5 and a cumulative dose of
cisplatin greater than 380 mg/m2 were associated with better OS.
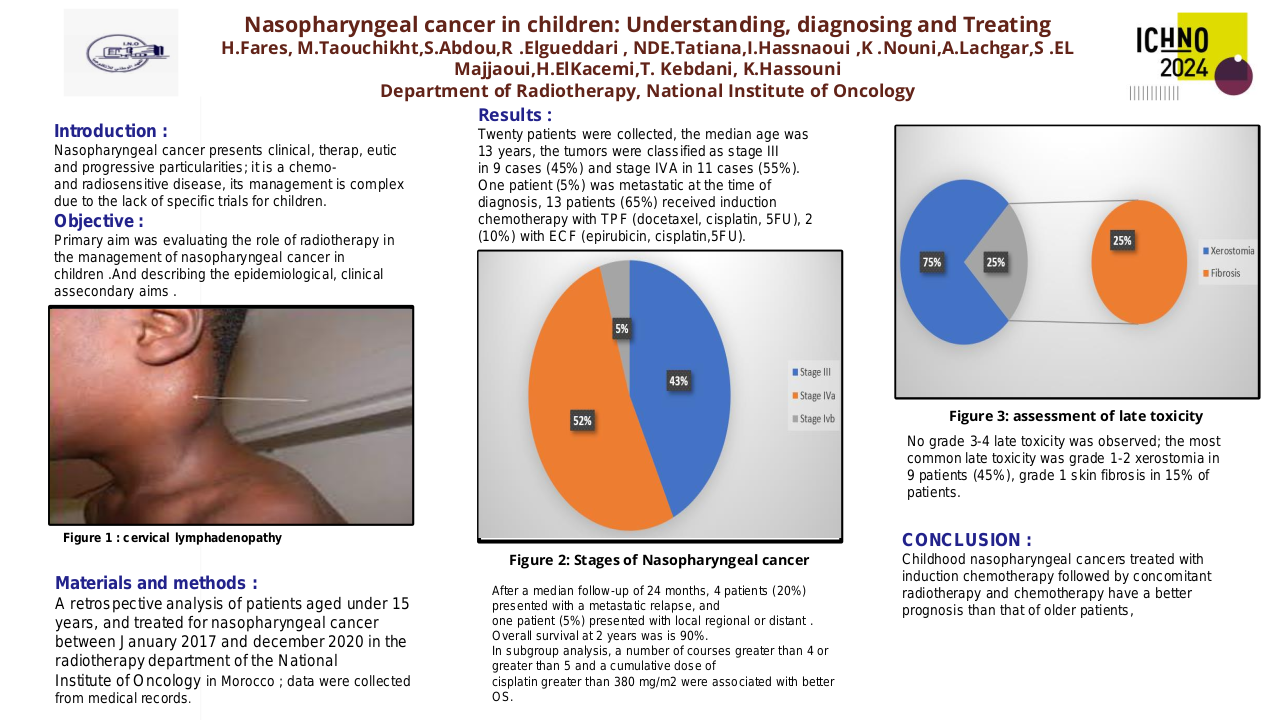
No grade 3-4 late toxicity was observed; the most common late toxicity was grade 1-2 xerostomia in
9 patients (45%), grade 1 skin fibrosis in 15% of patients.
Conclusion
Childhood nasopharyngeal cancers treated with induction chemotherapy followed by concomitant
radiotherapy and chemotherapy have a better prognosis than that of older patients,
however metastatic relapses remain frequent and determine the prognosis. The number of
chemotherapy courses as well as the cumulative dose of cisplatin seem to largely influence the
therapeutic results.