Concurrent chemoradiotherapy in the treatment of nasopharyngeal Carcinoma: data from 2018 to 2022
Purpose/Objective
Nasopharyngeal carcinoma is a malignant tumor that differs from other head and neck, it has a remarkable radiosensitivity and chemosensitivity, making concurrent chemoradiotherapy the standard treatment. Nasopharyngeal carcinoma is endemic in Morocco and North Africa.
The aim of this work is to evaluate the efficacy concomitant chemotherapy and conformational radiotherapy with intensity modulation in the treatment of patients with carcinoma of nasopharyngeal.
Material/Methods
The present retrospective study is an experience of the National Institute of Oncology in the curative treatment of nasopharyngeal carcinoma.
The study carried out 253 patients treated for non-metastatic nasopharyngeal cancer from January 2018 to December 2021.
We include in our study, patients who were histologically and radiology proven nasopharyngeal carcinoma disease and treated with only a concurrent chemoradiotherapy.
Results
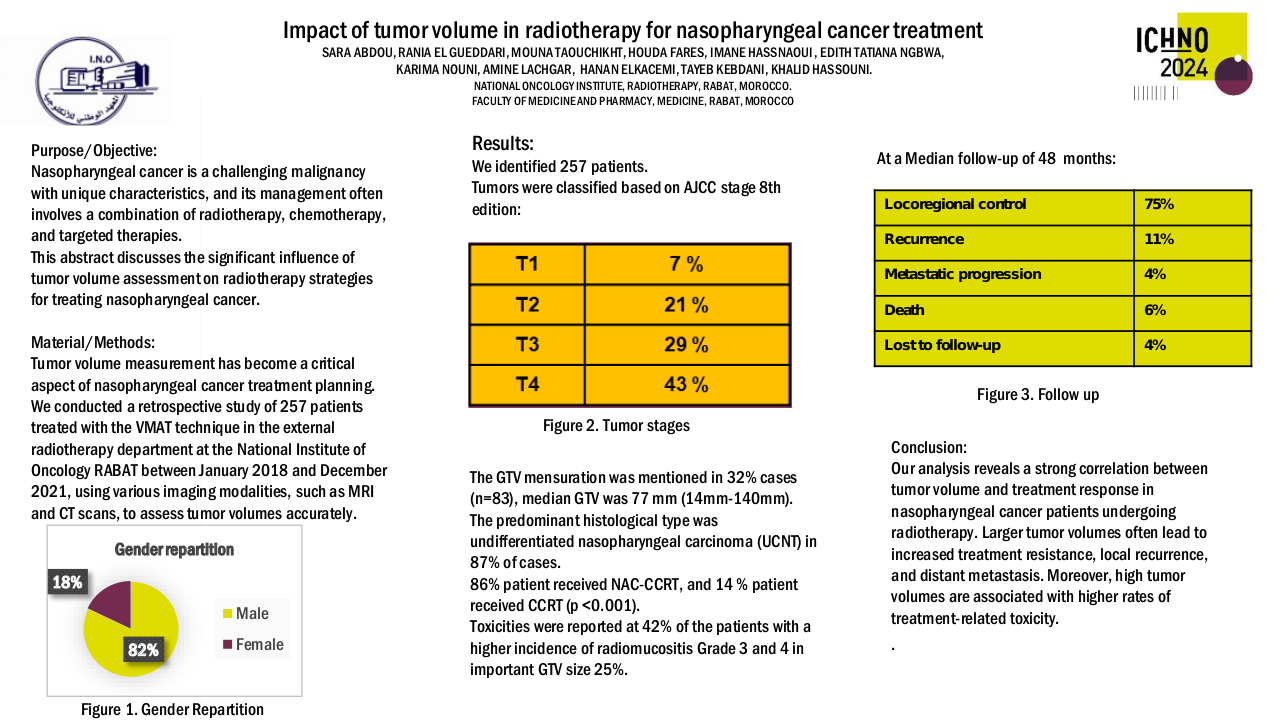
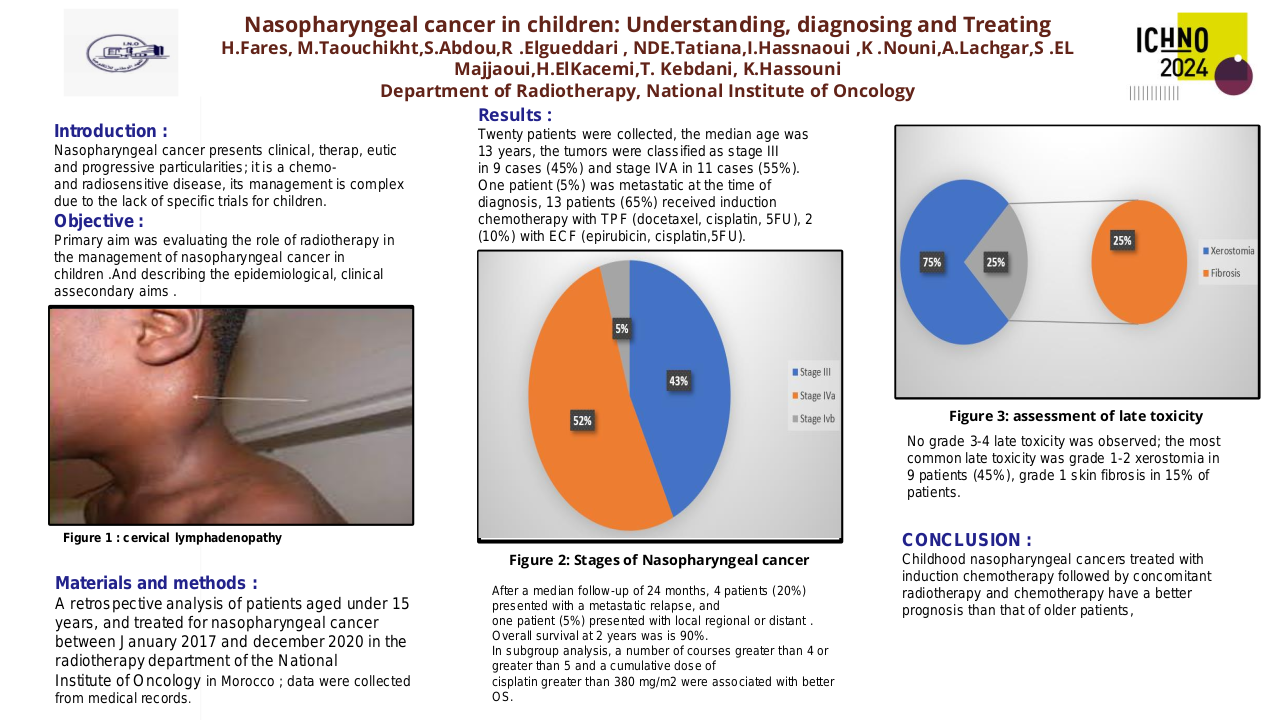
In our study, we included 80 patients who were only treated by a concurrent chemoradiotherapy.
The median age of our patients was 53.6 years with extremes between 19 years and 83 years.
33 patients were male and 45 were female.
25% of patients had co-morbidities, including 32 % with hypertension, 25 % with diabetes and two patients with a history of ischemic stroke. In our studies, 51% have been smoking for the last 10 years and the rest have never been smoking.
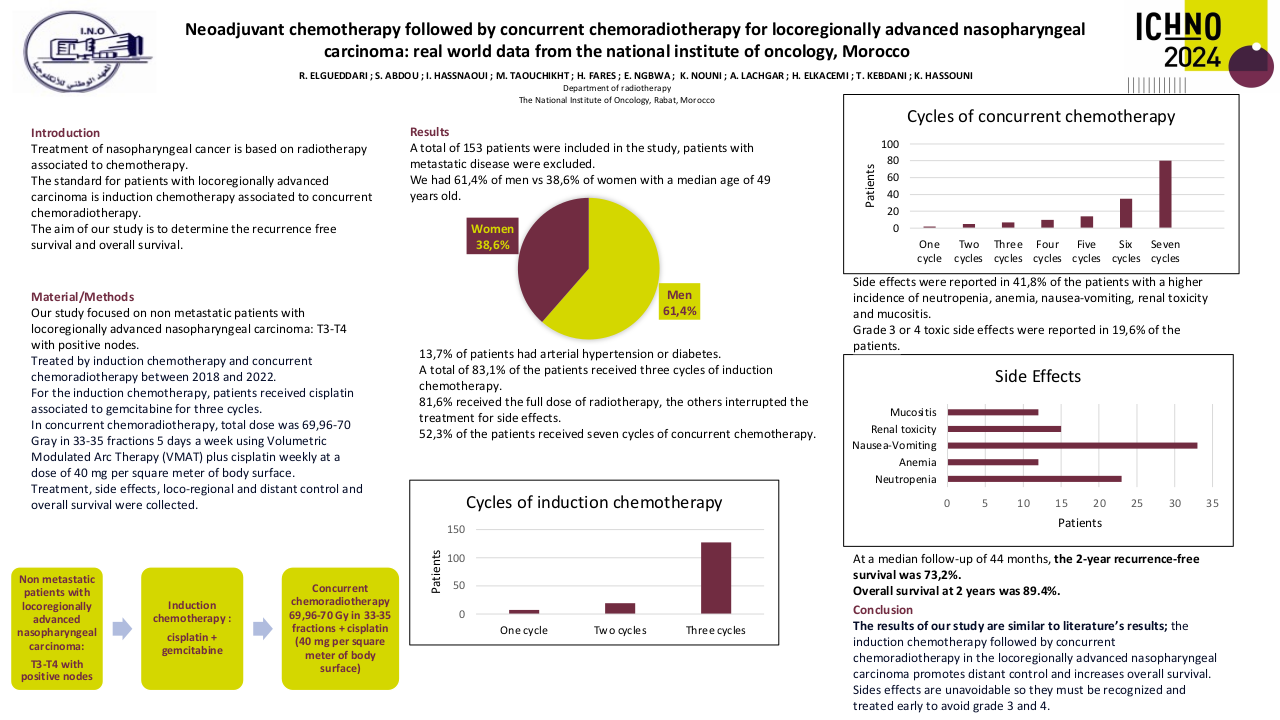
Thanks to pre-treatment IRM data, we were able to categorize patients according to the TNM classification.
11 patients had a T1 stage, 32 patients had a T2 stage, 20 had a T3 stage and 17 had a T4 stage.
Regarding to lymph nodes 16 patients had N0 stage, 31 had a N1 stage, 29 had a N2 stage and 4 patients had a N3 stage. 35% of the patients had a stage I, 38,75% had a stage II and 20 patients had stage III, respectively.
Patients were irradiated with a Volumetric Modulated Arc Therapy at the dose of 69.96 Gy, -70 Gy, 2.12 Gy-daily/fractions, 5 fractions per week. The average number of radiotherapy sessions was 33,3.
Concurrent Chemotherapy was administered weekly type cisplatin at a dose of 40 mg/m2.
The average dose of treatments was 4,75 sessions.
Both radiotherapy and chemotherapy have their share of toxicities.
Chemotherapy is mainly responsible for digestive toxicity, 70% of the patient reported nausea and emesis. Regarding to hematologic toxicity, 10 patients reported anemia, 20 patients developed a neutropenia and 5 patients developed a leucopenia.
Radiotherapy, on the other hand, 20% of the patient related a trismus, 50 % a hypoacusis and 2 patients presented a total deafness.
A complete tumor response was obtained in 68 patients, assessed by IRM DATA.
Only four patients presented a partial local response, then a progression. Two patients had a local relapse 2 years after the end of treatment and only 6 had a distant metastatic disease after the end of treatment.
Two patients died before starting their treatment, 3 others died one month after the end of the therapeutic protocol.
With a median follow up of 20 months, the overall survival and progression-free survival rates were 91.25% and 86.25 %, respectively.
Conclusion
Radiotherapy with modulated intensity and concurrent chemotherapy are effective, and well tolerated in the treatment of nasopharyngeal cancer.
To improve on current results, efforts are needed to evaluate and develop new therapeutic strategies
more effective and less toxic.