impact of tumor volume in radiotherapy for nasopharyngeal cancer treatment
Purpose/Objective
Nasopharyngeal cancer is a challenging malignancy with unique characteristics, and its management often involves a combination of radiotherapy, chemotherapy, and targeted therapies.
This abstract discusses the significant influence of tumor volume assessment on radiotherapy strategies for treating nasopharyngeal cancer.
Material/Methods
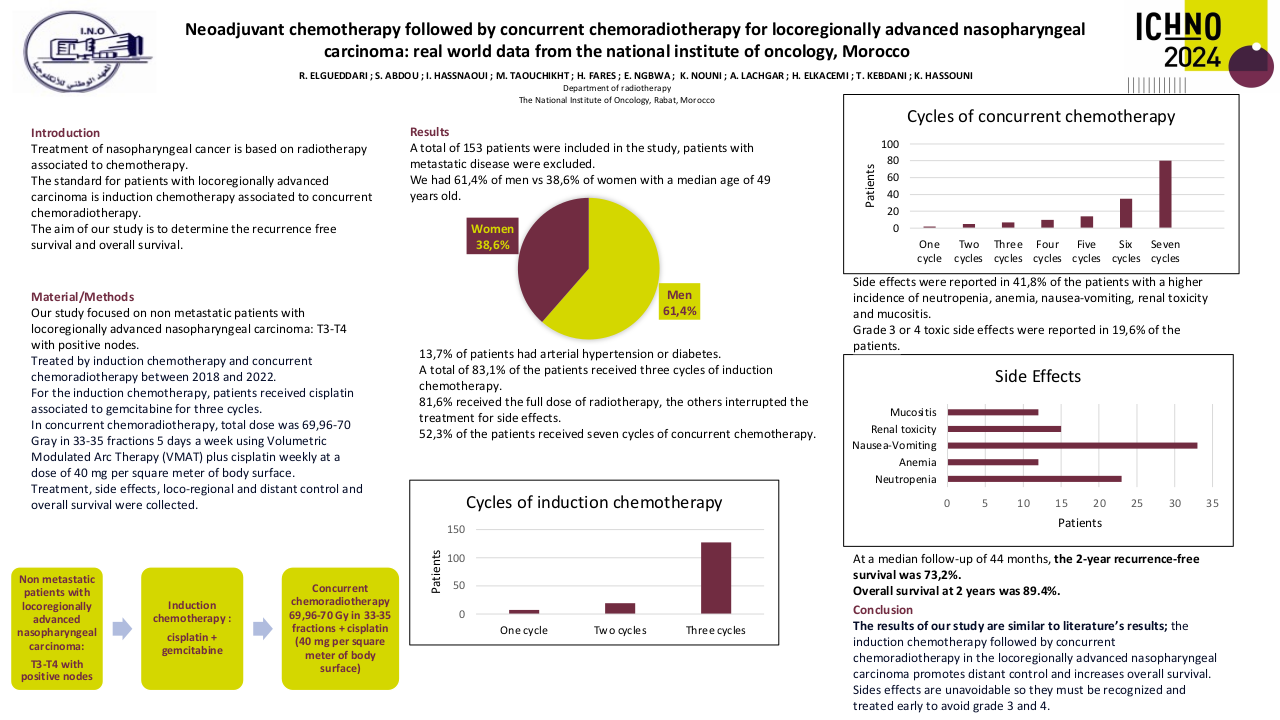
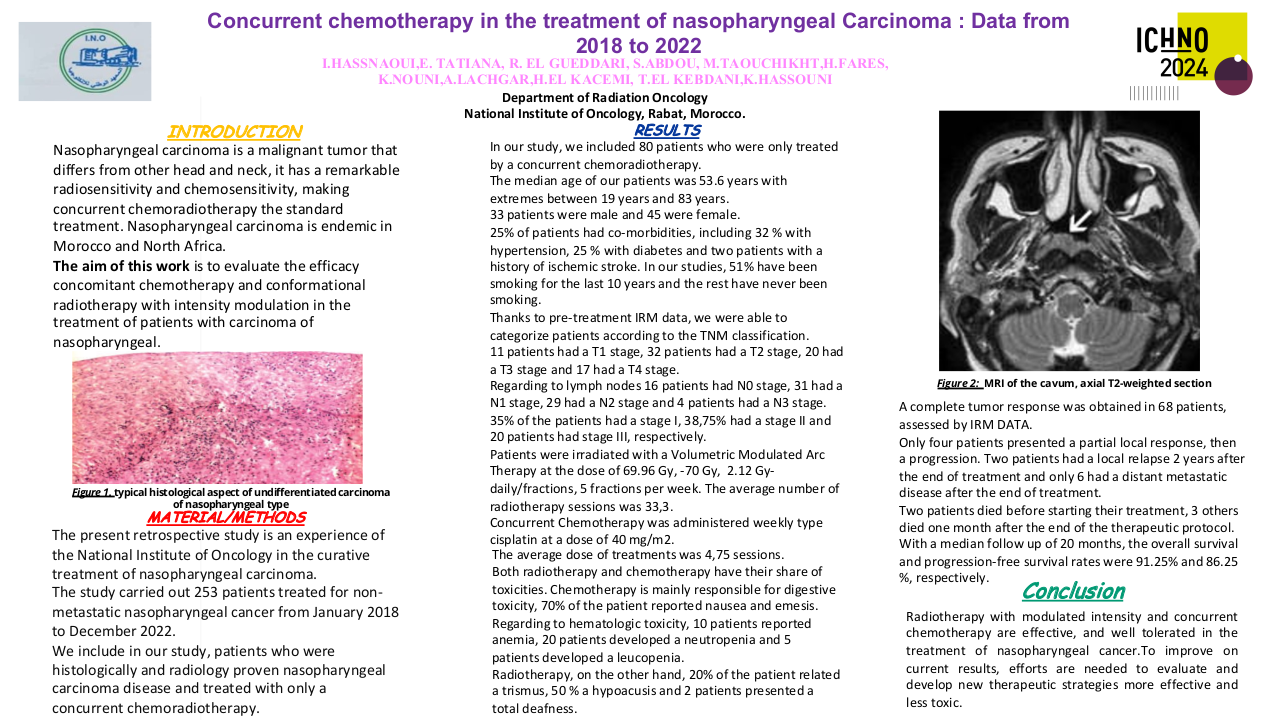
Tumor volume measurement has become a critical aspect of nasopharyngeal cancer treatment planning. We conducted a retrospective study of 257 patients treated with the VMAT technique in the external radiotherapy department at the National Institute of Oncology RABAT between January 2018 and December 2021, using various imaging modalities, such as MRI and CT scans, to assess tumor volumes accurately.
Results
We identified 257 patients.
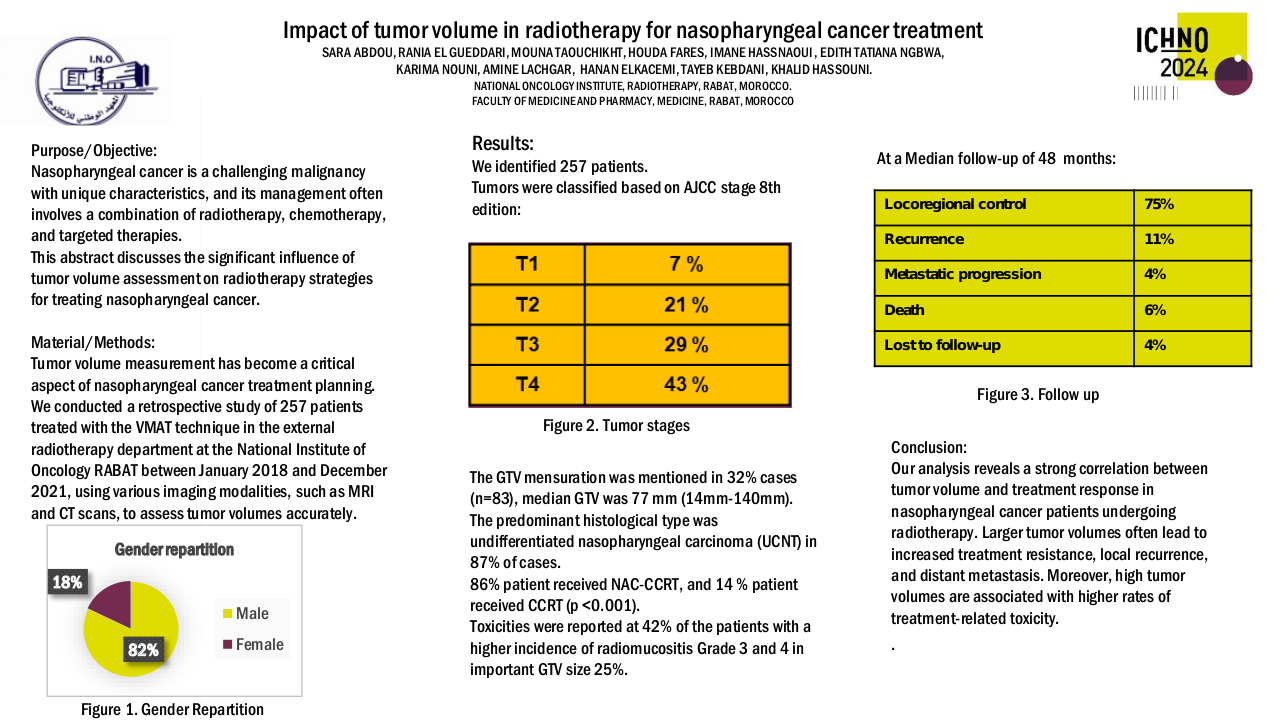
Sex repartition: 82% men and 18% women. Comorbidities were observed in 15% cases.
Tumors were classified as T1 in 7 %, T2 in 21 %, T3 in 29 %, and T4 in 43 % 21% based on AJCC stage 8th edition.
The GTV mensuration was mentioned in 32% cases (n=83), median GTV was 77 mm (14mm-140mm)
The predominant histological type was undifferentiated nasopharyngeal carcinoma (UCNT) in 87% of cases.
86% patient received NAC-CCRT, and 14 % patient received CCRT (p < 0.001).
Toxicities were reported at 42% of the patients with a higher incidence of radiomucositis Grade 3 and 4 in important GTV size 25%.
At a Median follow-up of 48 months, locoregional control was found in 75% of patients treated, with 11% of recurrence and 4% metastatic progression. 6% of patients died of their cancer and 4% were lost to follow-up
Conclusion
Our analysis reveals a strong correlation between tumor volume and treatment response in nasopharyngeal cancer patients undergoing radiotherapy. Larger tumor volumes often lead to increased treatment resistance, local recurrence, and distant metastasis. Moreover, high tumor volumes are associated with higher rates of treatment-related toxicity.