Head and neck re-irradiation: retrospective single institution study of 60 patients treated with curative intention.
Purpose/Objective
Radiotherapy (RT) plays a fundamental role in the definitive treatment of carcinoma of the head and neck cancer, but loco regional relapse happens up to 40% of the patients despite optimal initial multidisciplinary treatment, as well as second neoplasmstumors. Management of these scenarios is challenging, as re-treating an already irradiated field has a narrow balance between disease control benefit and toxicity risk. We aimed to provide data of outcomes in terms of disease control, survival and toxicity of re-irradiated patients, to facilitate selection and stratification of those who could benefit more.
Material/Methods
Retrospective analysis of patients with loco-regional relapse or second primary head and neck carcinomastumor who were re-irradiated between 2009 and-2023 in a previously irradiated field (≥50 Gy) using 3D or IMRT/VMAT, and conventional fractionation. Data about event-free survival (EFS), overall survival (OS), acute and chronic toxicity according to CTCAEv54 wereas collected from clinical reports.
Results
Sixty patients were re-irradiated. Most of them (78%) were male and 98% were ECOG 1-0. Mean age at diagnosis was 60 years (median 59y, range 51-67y). First diagnosis tumor histology was SCC in 94% of the patients, and was alsowas the most frequent histology (98%) for the second primary alsotumor. Most common site for both, first and second tumortumor was oral cavity (49% and 38%, respectively). Time between two RT treatments was at least 2 years in 63% of the patients, with no patients treated with less than 6 month6-month period (mean time to second RT 40.4 months, median 30.5 months, range range 19.5-54.5 months).
Most of the patient retreated underwent adjuvant RT (n=32, 58%), reaching a mean dose of 59.95Gy (70.00-48.40) in addition to concomitant chemotherapy (67%).
Re-irradiation was more mostly used in an adjuvant context (55%). Systemic concomitant treatment was 65%, with preference for triweekly regimens (34%). After second treatment, 58% of the patients had complete response, 40% had a partial response or stable disease, and only one patient progressedhad progression. Mean total dose for re-irradiation was 60 Gy (median 60 Gy, range 54-70 Gy). Only 22 of the re-irradiation treatment volumes included cervical areas. IMRT/VMAT was the preferred treatment technique (76%). All treatments were normo-fractionated treatments.
Mean follow up is was 2.7 years from the end of RT. All patients had at least a 6-months follow up. Acute toxicity after re- irradiation was very common (95%), occurring in 70% of the patients presented mucositis and 67% epithelitis. Long- term toxicity consisted of dysphagia (45 patients74), osteonecrosis (6 patients), fistula (5 patients), trismus (5 patients G3-4). Carotid rupture happened in one patient.
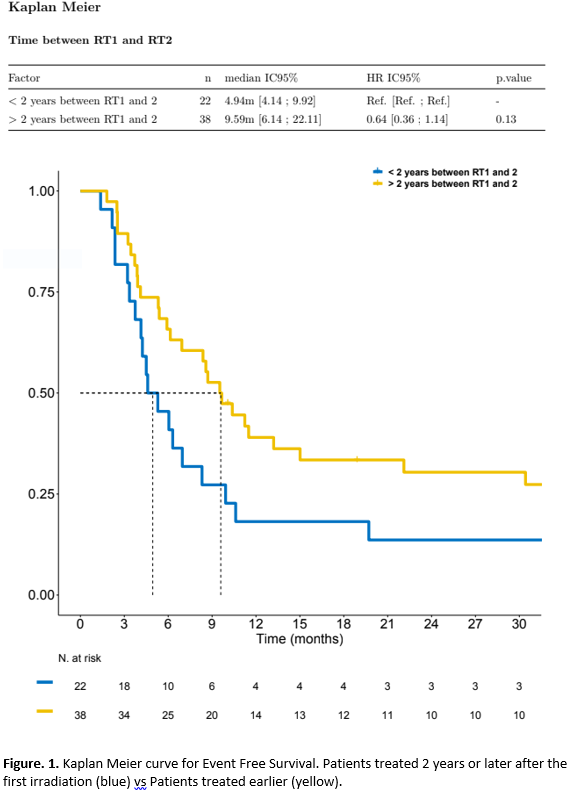
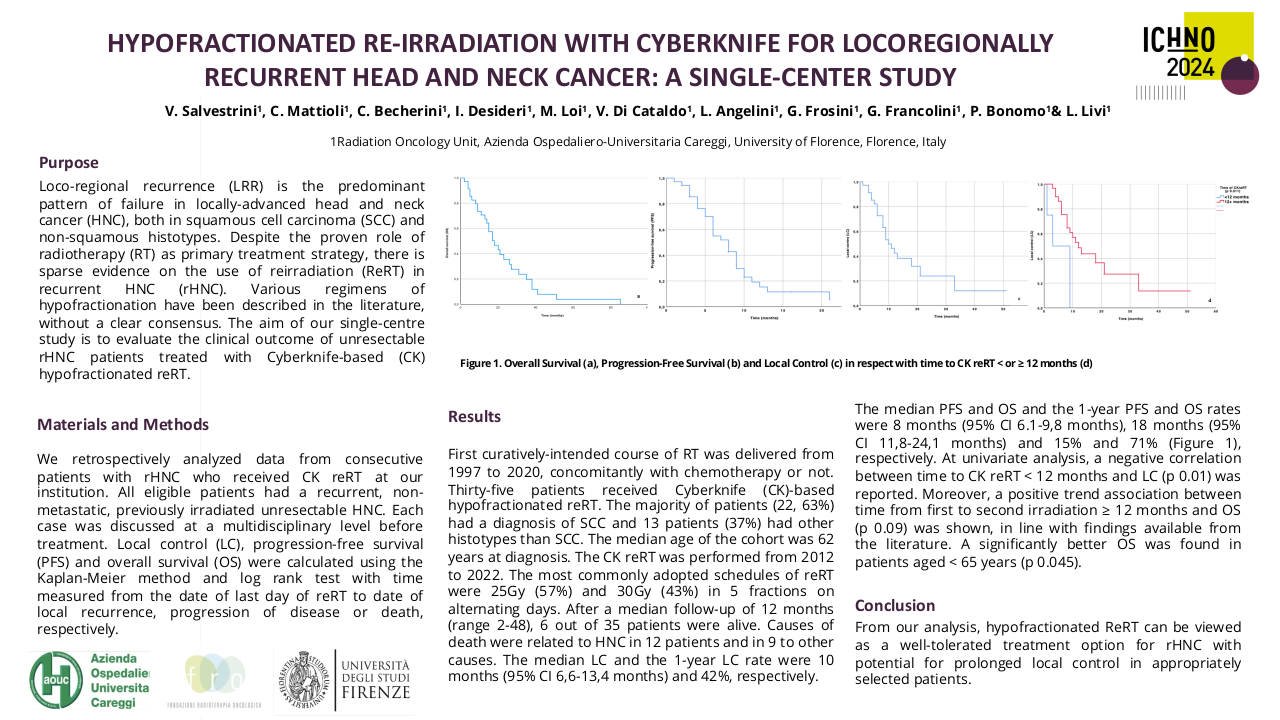
Mean time to progression was 20.4 months. Kaplan Kaplan-Meier analysis for event- free survival (EFS) shows better outcomes in patients who received re-irradiation at least 2 years after the first irradiation, with a median time to event of 9.59 6 months (95%CI 4.14-9.92m) compared with 4.94 months in patients who had earlier re-irradiation (95%CI 6.14-22.11m), with no statistically significant differences (Figure 1). No statistically significant differences in time to event according to total dose of re-irradiation were seen, as well as between patients with adjuvant or radical intention.
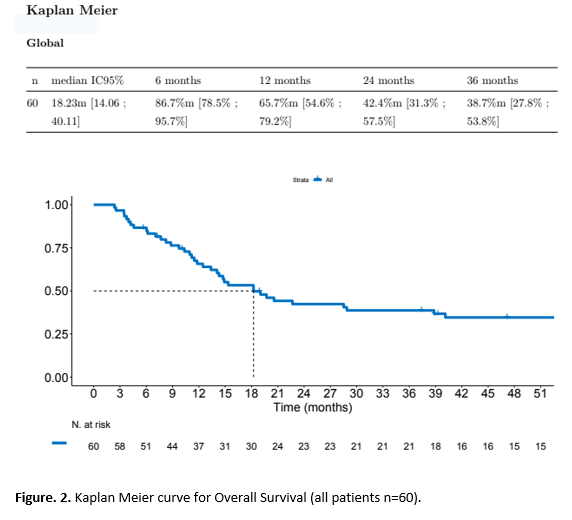
Median overall survival (OS) was 18.2 months (95%CI 14.061-40.1m) (Figure 2). At 51 months, 15 patients are still alive. OS is better in patients receiving RT more than 2 years after the first treatment (22.67 months vs 18.23 months), with differences maintained over the follow up. Patients who were treated with more than 50 Gy seem to have better median OS (19.7m vs 13.37m4m) without statistically significant differences.
Conclusion
Our analysis shows that patients with head and neck cancer with good performance status who undergo a re-irradiation treatment with curative intent present prolonged survival and disease control after the treatment, which seems benefited when second irradiation happens later than 2 years after the first course of RT, for both adjuvant and radical RT strategies.
1. Andratschke et al. European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus on re-irradiation: definition, reporting, and clinical decision making. Lancet Oncol 2022; 23: e469–78.2. Ward et al. Refining Patient Selection for Reirradiation of Head and Neck Squamous Carcinoma in the IMRT Era: A Multi-institution Cohort Study by the MIRI Collaborative. Int J Radiation Oncol Biol Phys 2018; 100 (3): 586-594.3. Ward et al. Retreatment of Recurrent or Second Primary Head and Neck Cancer After Prior Radiation: Executive Summary of the American Radium Society (ARS) Appropriate Use Criteria (AUC). Int J Radiat Oncol Biol Phys 2022; 15, 113 (4): 759-786.