Omitting postoperative contralateral radiotherapy in head and neck cancers. A single center report.
Purpose/Objective
Head and neck cancers (HNC) and their treatments with radiotherapy have been associated with acute and chronic toxicity mainly in relation with the volume of radiation.
Over the last years, the elective treatment of bilateral necks has been recommended by clinical practices guidelines. However, recently several retrospective and prospective studies have proposed the omission of the contralateral neck in radiation treatments, when lymphadenectomy is negative, to reduce the treatment volume and subsequently, to improve toxicity profiles in these patients without detrimental impact in overall survival.
We have sought the impact of omitting contralateral post-operative radiation therapy (PORT) by retrospective review of a cohort of patients in terms on Overall Survival (OS), Progression-Free Survival (PFS), Local Control (LC) and Contralateral Neck Recurrence (CLNR)
Material/Methods
Retrospective study of 31 patients diagnosed with squamous HNC treated with surgery complete bilateral neck dissection plus PORT in our centre between July 2019 and January 2023. PORT on the primary site was indicated in case of pT3-pT4 or in any case with <5mm surgical margin. Elective neck irradiation was administered in case of pN+ or pN0 if less tan 18 nodes were recovered,
The patients included presented a mean age of 63.5 years (44-81). Mean total length of treatment, measured from surgery until the end of radiotherapy was 3.48 months (2-5).
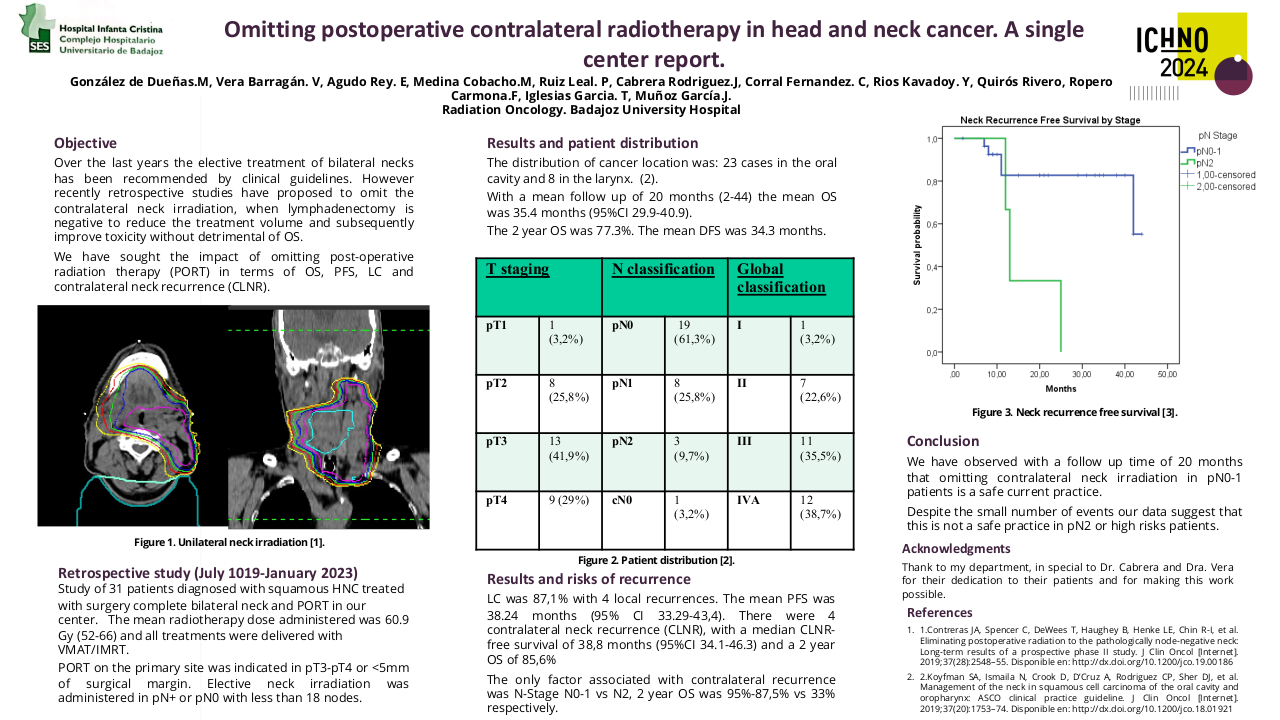
All the treatments were delivered with VMAT/IMRT on the postsurgical site of the primary tumour, and the ipsilateral elective neck.
The mean radiotherapy dose administered was 60.9 Gy (52-66), and the mean dose per fraction was 2.03 Gy (2-2.2). These doses were varied in relationship with status of the margins, ranged between 60-66Gy when the margins were affected. Minimum dose to pN+ neck was 60 Gy to involved node level, elective negative levels received 54Gy.
To analyse overall survival and time to progression free survival, Kaplan Meier curves was used. Log-rank test was used to analyse the difference in survival for categorical variables and the regression method for quantitative variables.
Results
The distribution of cancer location was: 23 cases in the oral cavity and 8 in the larynx. T staging: pT1 1 patient (3.2%), pT2 8 patients (25.8%), pT3 13 patients (41.9%), and pT4 9 patients (29%). N classification: pN0 19 patients (61.3%), pN1 8 patients (25.8%), pN2 3 patients (9.7%), and cN0 in 1 patient (3.2%). Global classification: stage I; 1 patient (3.2%), II; 7 patients (22.6%), III; 11 patients (35.5%), and IVA; 12 patients (38.7%).
Neck lymphadenectomy was radical in 4 patients (12.9%) and functional in 26 (83.9%). One patient did not undergo neck dissection during surgery for the primary but was included in the study. Mean number of lymph nodes recovered was 34.9 (8-90).
With a mean follow-up of 20 months (2-44) mean OS was 35.4 months (95%CI 29.9-40.9). The 2-year OS was 77.3%. The mean DFS was 34.3 months (95% CI 28.6-40.1), 2-year survival was 76%.
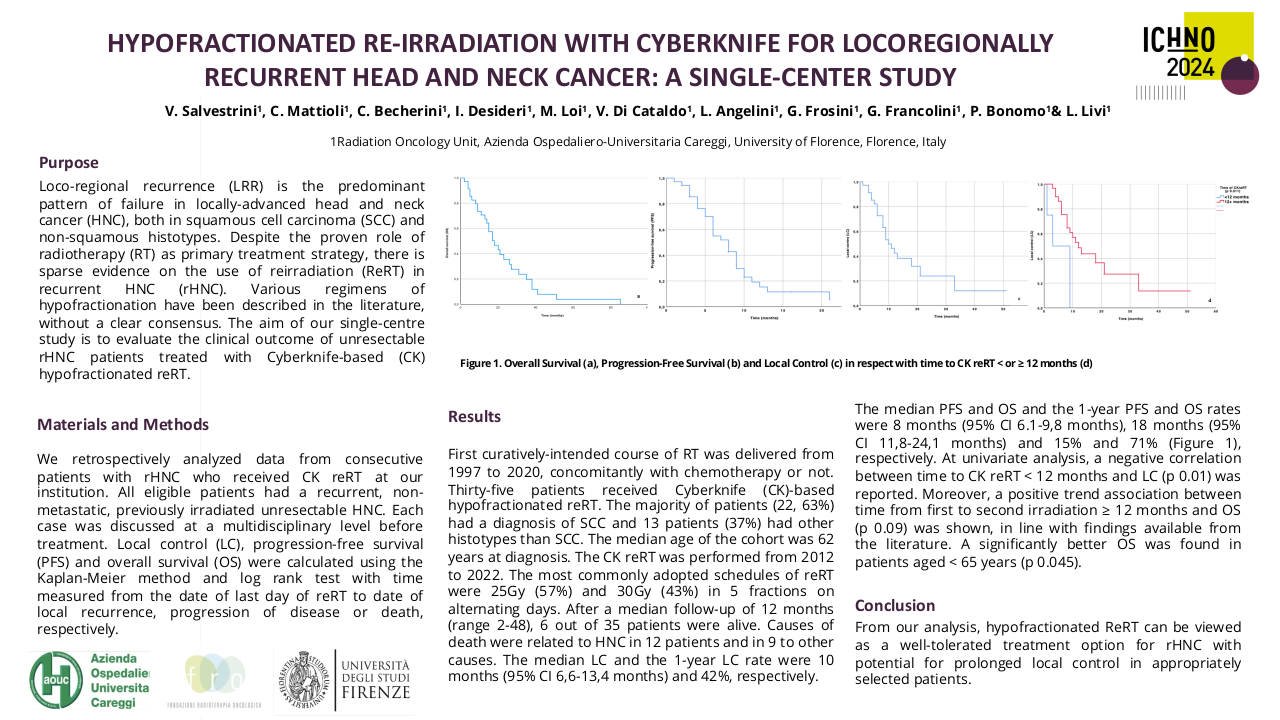
There was 4 local recurrences , 2-year actuarial LC was 87.1% with mean DFS 38.34 months (95%CI 33.29-43.4). There were 4 CLNR, with a median CLNR-free survival of 38.8 months (95%CI 34.1-43.6) 85.6% at 2 years.
The only factor associated with contralateral recurrence was N- Stage: N0-1 vs N2 2-year OS 95%-87.5% vs 33% respectively.
Median OS 42 vs13 months (p=0.02).
Conclusion
In conclusion, with a follow-up time of 20 months, we have observed that the omission of contralateral neck irradiation in patients with good prognosis factors as ipsilateral pN0-1 and bilateral neck lymphadenectomy is a safe current practice.
Despite being a study with a small number of events (n=4), our data suggest that omitting contralateral irradiation in pN2 patients is associated with a higher recurrence rate and worse survival. No other factors have been statistically significant with local recurrence rates neither OS.
1.Contreras JA, Spencer C, DeWees T, Haughey B, Henke LE, Chin R-I, et al. Eliminating postoperative radiation to the pathologically node-negative neck: Long-term results of a prospective phase II study. J Clin Oncol [Internet]. 2019;37(28):2548–55. Disponible en: http://dx.doi.org/10.1200/jco.19.001862.Koyfman SA, Ismaila N, Crook D, D’Cruz A, Rodriguez CP, Sher DJ, et al. Management of the neck in squamous cell carcinoma of the oral cavity and oropharynx: ASCO clinical practice guideline. J Clin Oncol [Internet]. 2019;37(20):1753–74. Disponible en: http://dx.doi.org/10.1200/jco.18.01921