Point Of Care Ultrasound (POCUS) in Tracheostomy in Head and Neck Cancer : A Prospective Study.
Purpose/Objective
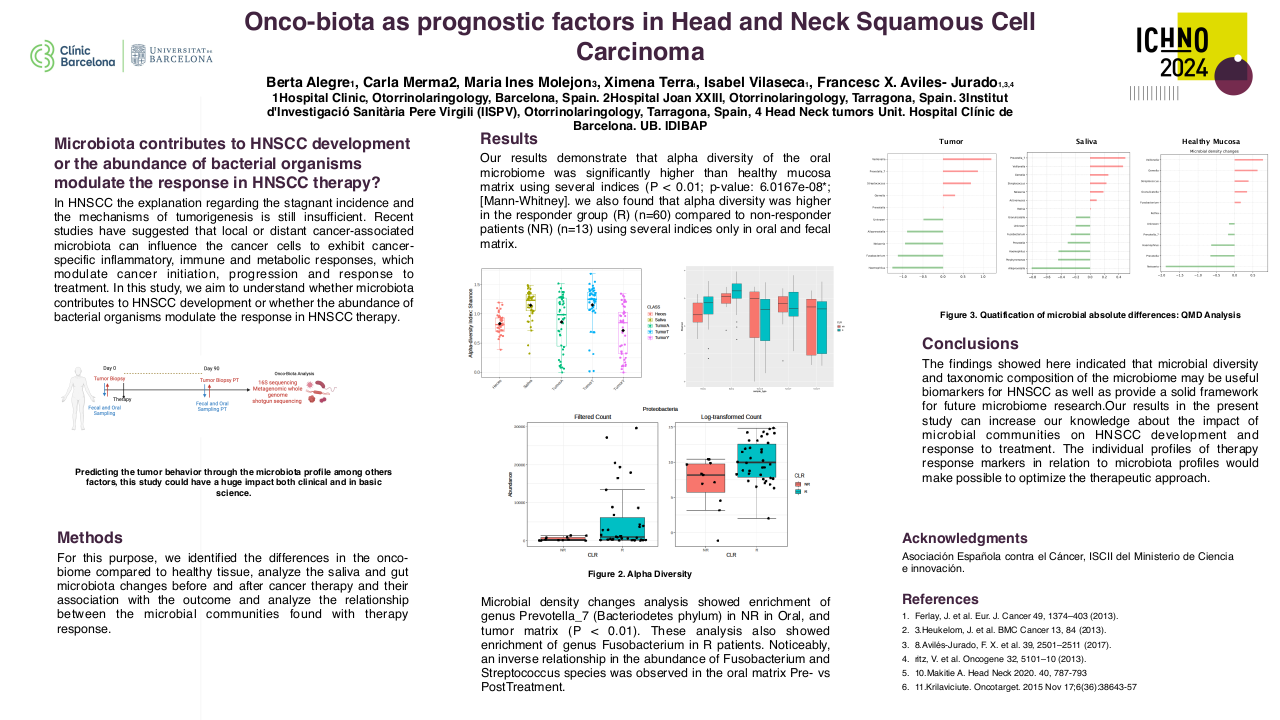
In a high volume, tertiary care oncology centre in India, tracheostomy is a relatively common emergency procedure that is done to relieve airway obstruction.1 However, in presence of bulky neck nodes, deviated trachea, post radiation fibrosis, lymphedema and inability to position the patient adequately; it may lead to difficulty in palpating and localizing the trachea.2 Furthermore, disease related factors like subglottic extension and extra laryngeal extension may distort the airway anatomy , and may complicate tracheostomy tube insertion.
Purpose:
1.To study the role of Point Of Care Ultrasound (POCUS) in head and neck cancer patients undergoing tracheostomy.
Objectives:
- To study the role of POCUS in localising the trachea in head and neck cancer patients undergoing tracheostomy.
- To study the role of POCUS in localising the level of tracheotomy in head and neck cancer patients undergoing tracheostomy.
Material/Methods
The study was conducted as a prospective cross sectional study for diagnostic accuracy in the Department of Head and Neck Oncology in Dr B Borooah Cancer Institute, Guwahati, India. It was conducted over 8 months from March 2023 to September 2023. All patients, above 18 years of age, undergoing tracheostomy due to upper airway obstruction or bleeding due to head and neck malignancy were included in the study. Patients undergoing elective tracheostomy as a part of a major surgical procedure, like free flap, large tongue defects; or for prolonged intubation were excluded from the study. In addition, hemodynamically unstable patients in severe respiratory distress/stridor due to head and neck malignancies were excluded as POCUS is still in an experimental phase for upper airway evaluation.
A focused ultrasound of the neck was performed by same two surgeons, who have received training for airway ultrasound; and was supervised by a critical care physician. The limits of examination included hyoid to suprasternal notch vertically. The POCUS focused on the following parameters:
- Location of the trachea and midline
- Estimating the thickness of any abnormal soft tissue overlying the trachea (from skin to anterior surface of trachea)
- Estimating the level of tracheostomy or tracheal cut, by localising any subglottic disease with tracheal extension
- Location of cricothyroid membrane
- Identifying any tracheal luminal narrowing or compression
- Identification of any abnormal vessels The time taken for the assessment, and complications following or during the tracheostomy was recorded and compared with intraoperative findings and CT findings using appropriate tests of statistical significance. Tracheostomies were further classified into primary and revision tracheostomies; and post irradiation status of the neck.
Results
Out of the 65 tracheostomies, landmarks were clearly identifiable in 34 studies. Difficult tracheostomy groups were identified as:
- Anterior neck mass >4 cm with inability to palpate trachea underneath (4)
- Post irradiated neck with fibrosis with inability to palpate the trachea/ inadequate neck extension (22)
- Bulky nodal disease reaching midline, with or without tracheal deviation/luminal compromise (7)
- Abnormal large vessels reaching midline (1)
- Tracheal extension of disease with or without luminal compromise (2)
Overlapping features were also noted across these 5 groups.
In patients with identifiable landmarks, there was no statistically significant difference in the outcome of successful tube insertion with or without POCUS (p=0.94). Sensitivity of POCUS to localise the trachea in post irradiated neck was 100%. In patients with anterior neck mass, POCUS identified the point of least dissection to reach the tracheal wall in all 4 patients. Similarly, POCUS identified the position of trachea and site of tracheotomy in 6 out of 7 patients (85.71%) with bulky nodal disease.
Tracheotomy level could be guided by POCUS in two scenarios:
- To identify the ring below the tracheal extension
- To select candidates for high tracheostomy if any gross extralaryngeal extension was identified (possible candidate for total laryngectomy). A total of 12 cases were revision tracheostomies. POCUS aided tracheostomy identified the trachea in all cases even in presence of granulations and fibrosis. The sensitivity to correctly identify the level of tracheotomy was 91.67%
Conclusion
POCUS can be immensely useful in head and neck cancer patients presenting in a “cannot intubate, cannot oxygenate” situation, with distorted neck anatomy. This is a fairly commonly encountered situation in the Indian subcontinent. POCUS can aid in difficult anticipated tracheostomy in localizing the trachea and planning of the surgery.
1. Chen, K., Varon, J., & Wenker, O. C. (1998). Malignant Airway Obstruction: Recognition and Management. The Journal of Emergency Medicine, 16(1), 83–92. doi:10.1016/s0736-4679(97)00245-x.2.Hathiram, Bachi & Rai, Reema & Watve, Parag & Khattar, Vicky. (2010). Tracheostomy in Head and Neck Cancers. Otorhinolaryngology Clinics An International Journal. 2. 53-60.10.5005/jp-journals-10003-1017.