Dose prescription variability in Oropharynx Cancer Radiotherapy
Purpose/Objective
Radiotherapy treatment planning hinges on a critical factor: the prescribed dose. Surprisingly, no consistent, standardised global approach to interpreting this prescription exists. This study aimed to examine and illustrate the variations in prescribed doses for the same treatment across North European and North American centres.
Material/Methods
The study analysed consecutively treated oropharynx cancer patients from six globally recognised radiotherapy departments. The criteria for inclusion encompassed curative IMRT or VMAT radiotherapy administered in 2017 or later. These centres were divided into three North American and three North European centres.
Dose-volume histogram (DVH) data were extracted from the local treatment planning system for the Gross Tumour Volume (GTV), the high-dose Clinical Target Volume (CTV), and Planning Target Volume (PTV) for each patient. The DVH was sampled in 1 cGy dose bins across the 0 to 100 Gy range.
All DVHs were scaled to a standard prescription of 70 Gy delivered in 35 fractions to facilitate straightforward comparisons across centres. No biological corrections were applied.
For the three target volumes (GTV, CTV, PTV), we extracted and compared metrics such as D95% (Dose to 95% of the volume), D98%, D99%, V95% (Volume receiving 95% of the prescription dose), V105%, and V107%. We visually compared these metrics and conducted statistical testing using the Mann-Whitney U-test.
Results
Our study encompassed 1,375 patients treated across six centres, revealing a spectrum of 38 different dose prescriptions, ranging from 55 Gy in 20 to 70 Gy in 35 fractions.
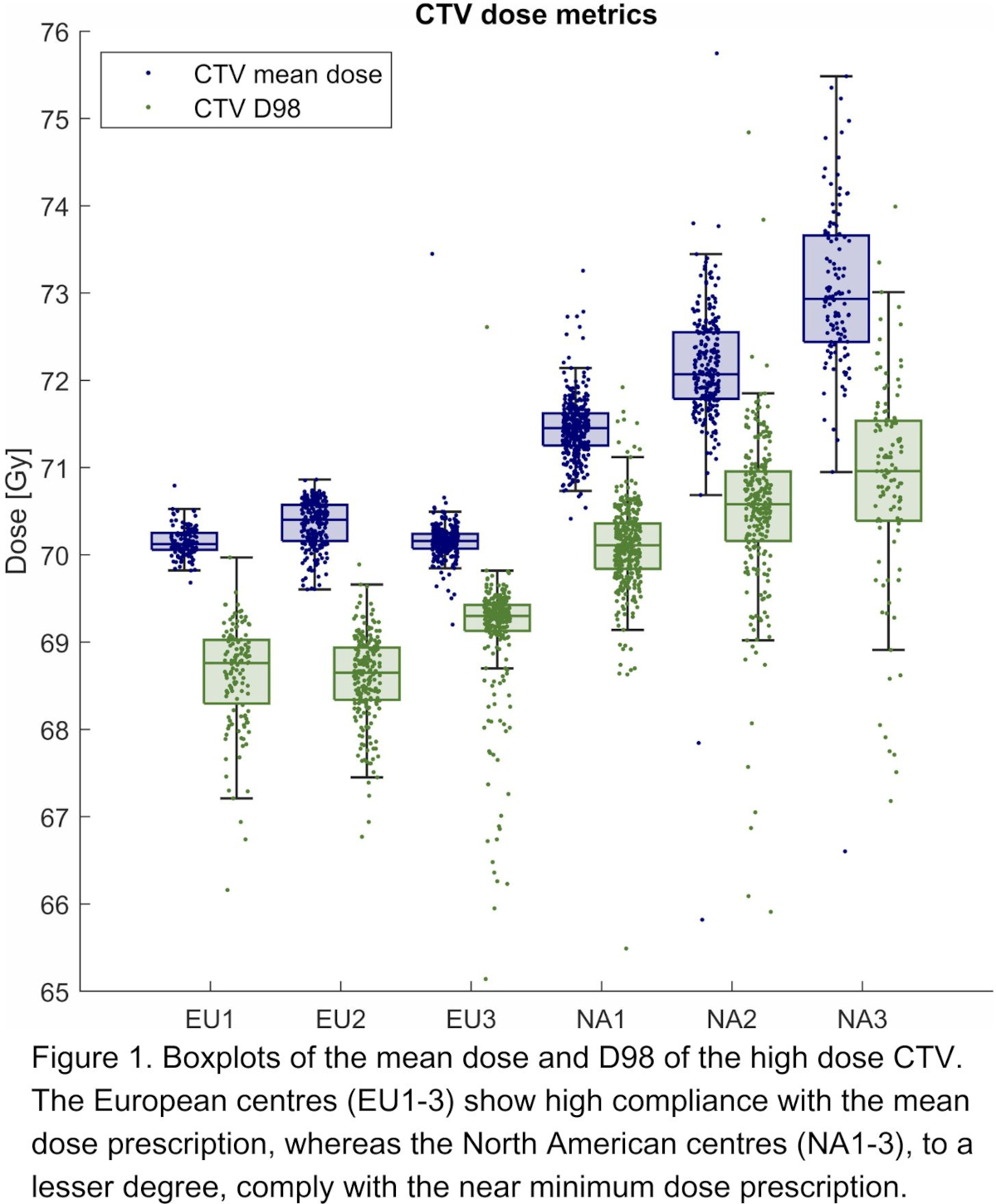
When normalised to 70 Gy, the median mean CTV dose exhibited a 4% difference, ranging from 70.12 Gy to 72.93 Gy across centres. Notably, the three European centres showed a high consistency, deviating by only 0.4%, while the three North American centres showed a slight variation within 2%. Figure 1 presents the mean CTV dose and the D98% boxplots. The interquartile range (IQR) for the mean CTV dose from 0.17 Gy to 1.22 Gy, with European centres showing the smallest IQR.
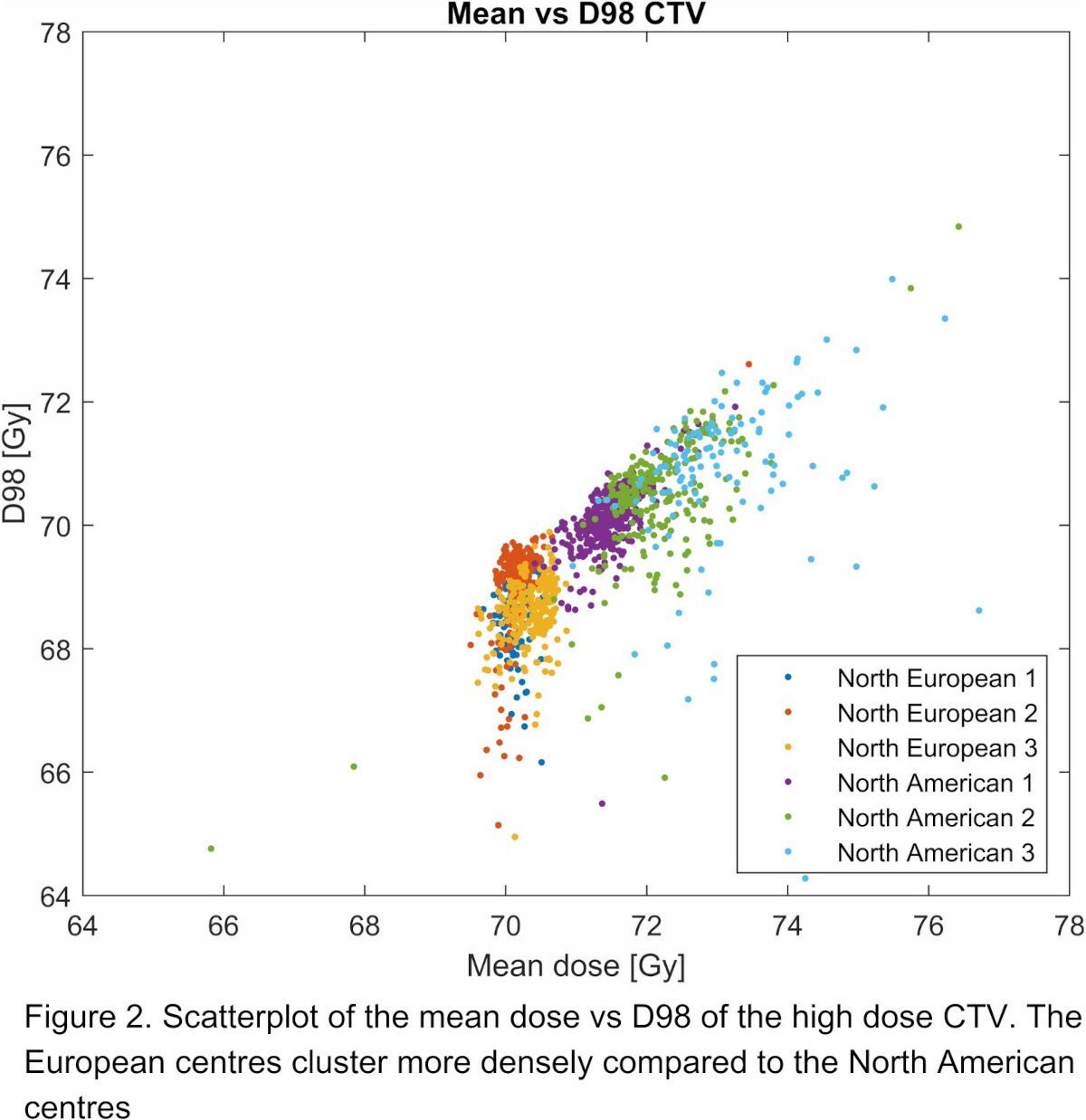
Examining the near-minimum CTV doses (D98% of CTV), we observed a range from 68.65 Gy to 70.96 Gy, with an IQR from 0.30 Gy to 1.15 Gy. A scatter plot of CTV mean dose against CTV D98% revealed distinct clusters for each of the six centres (Figure 2). Notably, the European centres cluster more densely compared to the North American centres.
The variation in prescribed doses for the same treatment regimen poses a significant challenge. Clinical interpretation of 70 Gy varies widely between centres and is influenced by each centre's individual experience, which, in turn, impacts the interpretation of published results. European centres primarily adhere to the ICRU dose prescription, targeting the median CTV dose. Conversely, North American centres tend to prescribe based on the minimum dose to the CTV or, in some cases, the PTV, as outlined in various RTOG protocols.
Conclusion
Our study underscores that prescribing a dose of 70 Gy in 35 fractions for standard oropharynx cancer patients results in substantial variations in mean and near-minimum CTV doses. These dose prescription discrepancies significantly impact the interpretation of clinical trial outcomes comparison. Furthermore, this significant dosimetric variability has important implications for dose de-escalation strategies for HPV+ oropharynx cancer treatment.