A five-year experience of intensity modulated radiotherapy in nasopharyngeal carcinomas in Tunisia
Purpose/Objective
Intensity modulated radiation (IMRT) technique, associated with induction chemotherapy (IC) and/or concomitant chemotherapy (CC) is actually the recommended treatment modality for nasopharyngeal carcinomas (NPC). The aim of this study was to evaluate the therapeutic results and the patterns of relapse with this treatment protocol.
Material/Methods
A retrospective monocentric study of 145 patients with NPC treated between June 2016 and July 2021. All patients received IMRT with integrated simultaneous boost (SIB) of 33 daily fractions at a dose of 69.96 Gy for high-risk volume, 60 Gy for intermediate risk volume and 54 Gy for low-risk volume. High risk volume dose was 66.5 Gy in children.
Survival analysis was performed according to Kaplan-Meier method and Log-rank test was used to compare factors that may influence survivals.
Results
Median age was 48 years (11-80) with a sex ratio of 2.9. One hundred-twenty tumors (82.7%) were classified as stages III-IV according to the 2017 UICC TNM classification. Ten patients (6.9%) were metastatic at diagnosis. One hundred-thirty-five patients (93.1%) received IC, 104 of which (77%) were TPF-based (taxanes, cisplatin and 5 fluoro-uracil). One hundred-thirty-eight patients (95.2%) received CC, mostly cisplatin in 134 cases (97%).
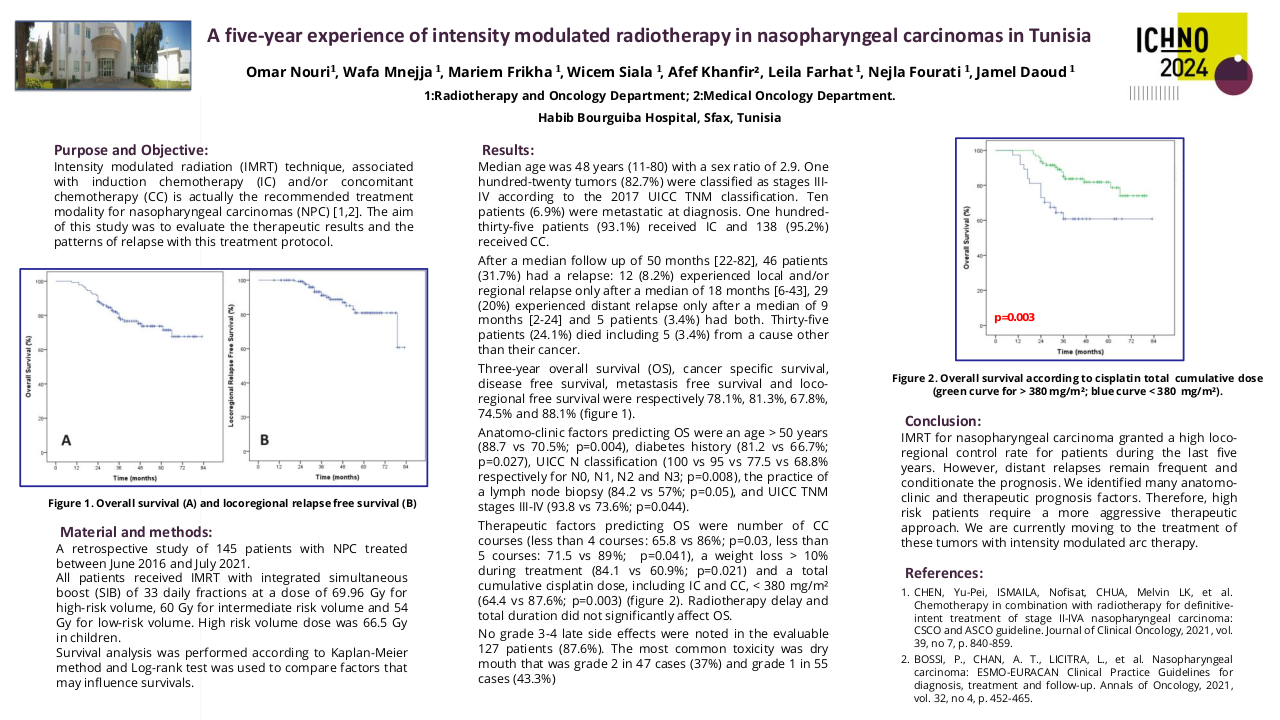
After a median follow up of 56 months [28-86], 46 patients (31.7%) had a relapse: 12 (8.2%) experienced local and/or regional relapse after a median of 18 months [6-43], 29 (20%) experienced distant relapse after a median of 9 months [2-24] and 5 patients (3.4%) had both. Thirty-five patients (24.1%) died including 5 (3.4%) from a cause other than their cancer. Three-year overall survival (OS), cancer specific survival, disease free survival, metastasis free survival and loco-regional free survival were respectively 78.1%, 81.3%, 67.8%, 74.5% and 88.1%.
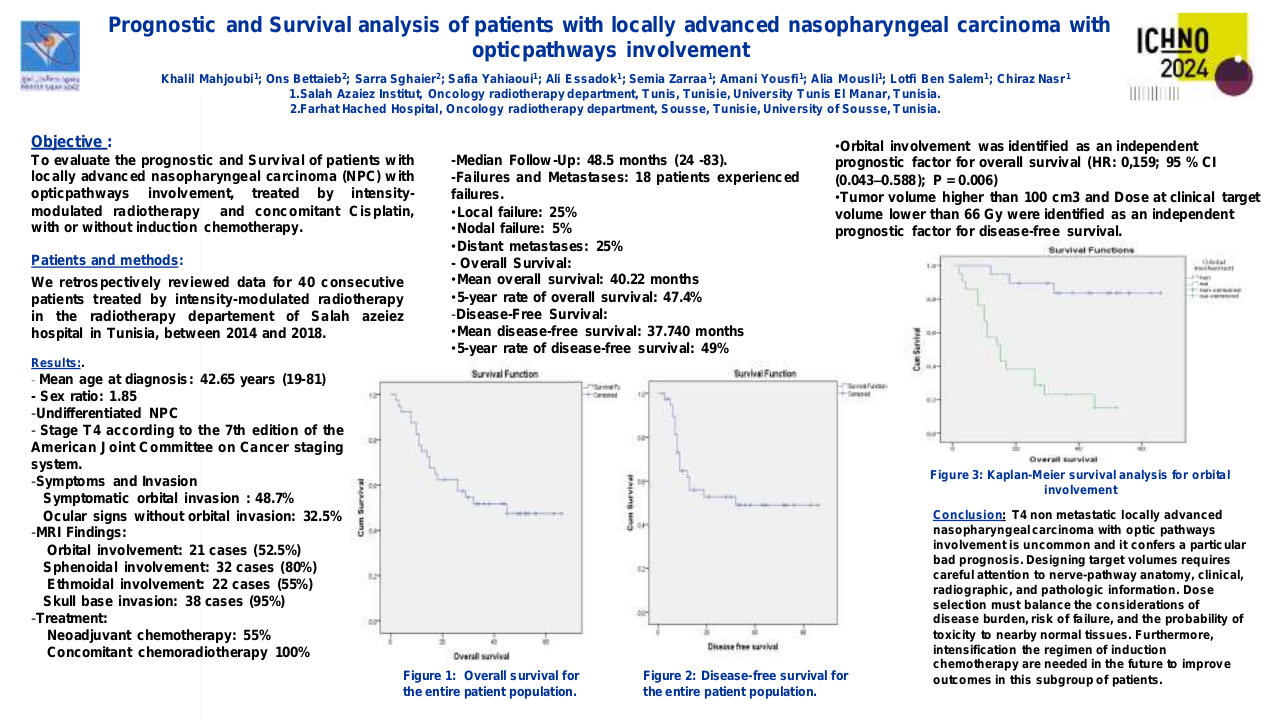
Anatomo-clinic factors predicting OS were an age > 50 years (88.7 vs 70.5%; p=0.004), diabetes history (81.2 vs 66.7%; p=0.027), UICC N classification (100 vs 95 vs 77.5 vs 68.8% respectively for N0, N1, N2 and N3; p=0.008), the practice of a lymph node biopsy (84.2 vs 57%; p=0.05), and UICC TNM stages III-IV (93.8 vs 73.6% respectively for stage I-II vs III-IV; p=0.044). Therapeutic factors predicting OS were number of CC courses (less than 4 courses: 65.8 vs 86%; p=0.03, less than 5 courses: 71.5 vs 89%; p=0.041), a weight loss > 10% during treatment (84.1 vs 60.9%; p=0.021) and a total cumulative cisplatin dose, including IC and CC, < 380 mg/m² (64.4 vs 87.6%; p=0.003). Radiotherapy delay and total duration did not significantly affect OS.
No grade 3-4 late side effects were noted in the evaluable 127 patients (87.6%). The most common toxicity was dry mouth that was grade 2 in 47 cases (37%) and grade 1 in 55 cases (43.3%).
Conclusion
IMRT for nasopharyngeal carcinoma granted a high loco-regional control rate for patients during the last five years. However, distant relapses remain frequent and conditionate the prognosis. We identified many anatomo-clinic and therapeutic prognosis factors. Therefore, high risk patients require a more aggressive therapeutic approach such as radiotherapy dose escalation or adding adjuvant chemotherapy.