PET CT response outcomes in curatively treated oropharyngeal SCC with bulky N3 neck disease
Purpose/Objective
PET CT scans are used to assess the response following curative intent chemoradiotherapy (CRT) or radiotherapy (RT) for oropharyngeal SCC (OPSCC) 12 weeks after completion of treatment. In the practice changing PETNECK randomised controlled trial, there were 17 patients with N3 neck disease (9 who underwent PET CT surveillance and 8 had planned neck dissections) and in another study (Beyond PETNECK) there were 10 patients. There is little data regarding outcomes following treatment for bulky N3 neck disease. We reviewed our experience of treating patients with bulky N3 neck disease (nodes >6cm, as per TNM7 staging) and their outcomes.
Material/Methods
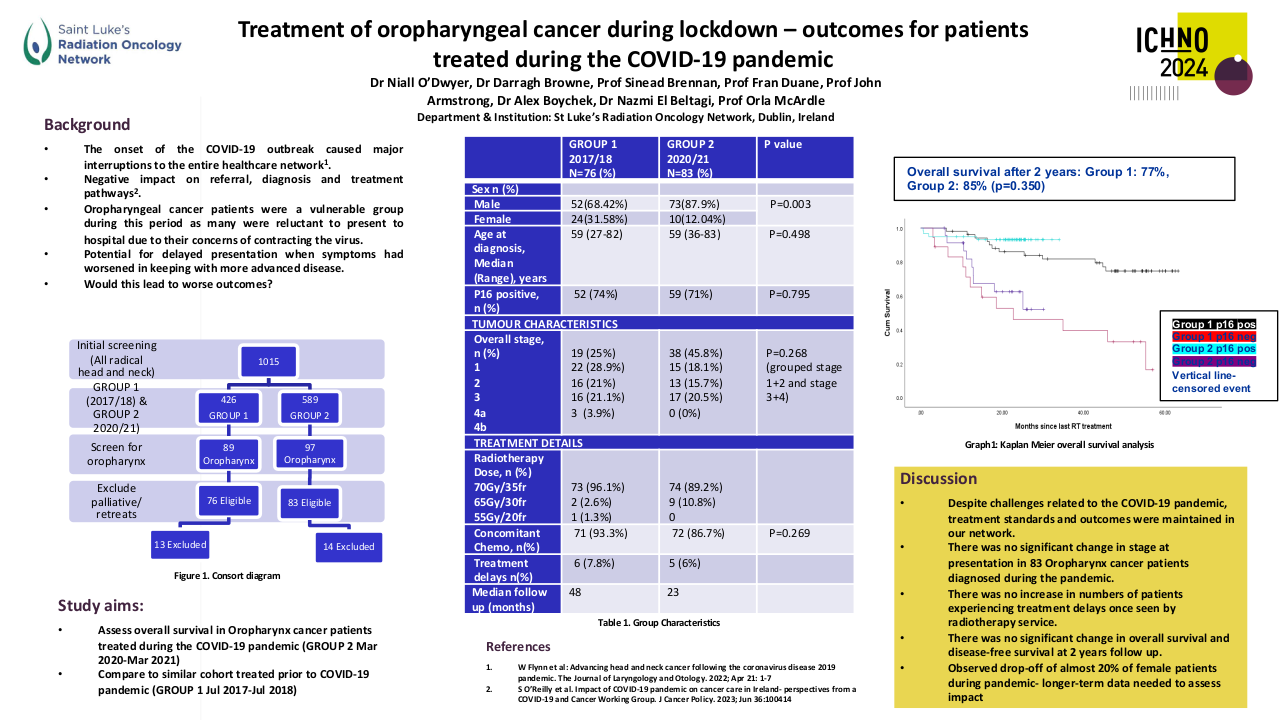
Patients who had PET CT scans following definitive treatment for OPSCC between 2016 – 2022 in South East Wales were reviewed. 260 patients fulfilled the criteria, of which there were 20 patients with N3 neck disease. Patient demographics, treatment details and PET CT outcomes were collated and analysed.
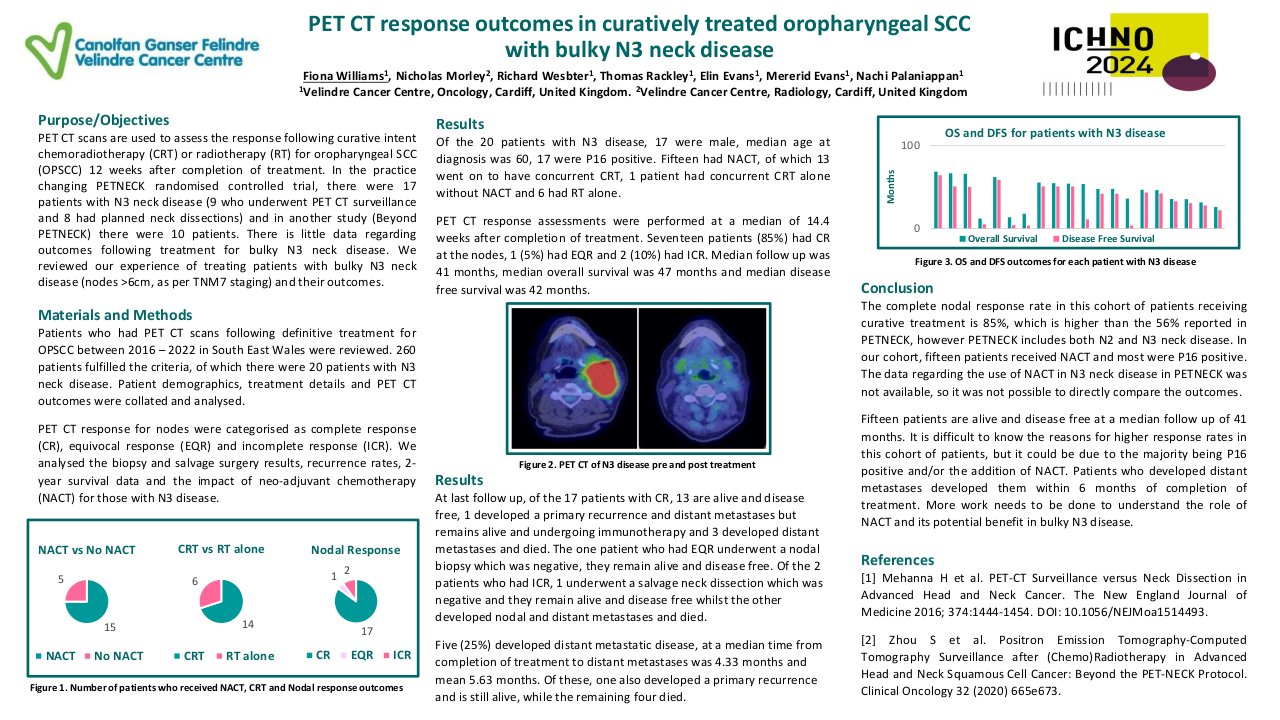
PET CT response for nodes were categorised as complete response (CR), equivocal response (EQR) and incomplete response (ICR). We analysed the biopsy and salvage surgery results, recurrence rates, 2-year survival data and the impact of neo-adjuvant chemotherapy (NACT) for those with N3 disease.
Results
Of the 20 patients with N3 disease, 17 were male, median age at diagnosis was 60, 17 were P16 positive. Fifteen had NACT, of which 13 went on to have concurrent CRT, 1 patient had concurrent CRT alone without NACT and 6 had RT alone.
PET CT response assessments were performed at a median of 14.4 weeks after completion of treatment. Seventeen patients (85%) had CR at the nodes, 1 (5%) had EQR and 2 (10%) had ICR. Median follow up was 41 months, median overall survival was 47 months and median disease free survival was 42 months.
At last follow up, of the 17 patients with CR, 13 are alive and disease free, 1 developed a primary recurrence and distant metastases but remains alive and undergoing immunotherapy and 3 developed distant metastases and died. The one patient who had EQR underwent a nodal biopsy which was negative, they remain alive and disease free. Of the 2 patients who had ICR, 1 underwent a salvage neck dissection which was negative and they remain alive and disease free whilst the other developed nodal and distant metastases and died.
Five (25%) developed distant metastatic disease, at a median time from completion of treatment to distant metastases was 4.33 months and mean 5.63 months. Of these, one also developed a primary recurrence and is still alive, while the remaining four died.
Conclusion
The complete nodal response rate in this cohort of patients receiving curative treatment is 85%, which is higher than the 56% reported in PETNECK, however PETNECK includes both N2 and N3 neck disease. In our cohort, fifteen patients received NACT and most were P16 positive. The data regarding the use of NACT in N3 neck disease in PETNECK was not available, so it was not possible to directly compare the outcomes.
Fifteen patients are alive and disease free at a median follow up of 41 months. It is difficult to know the reasons for higher response rates in this cohort of patients, but it could be due to the majority being P16 positive and/or the addition of NACT. Patients who developed distant metastases developed them within 6 months of completion of treatment. More work needs to be done to understand the role of NACT and its potential benefit in bulky N3 disease.
[1] Mehanna H et al. PET-CT Surveillance versus Neck Dissection in Advanced Head and Neck Cancer. The New England Journal of Medicine 2016; 374:1444-1454. DOI: 10.1056/NEJMoa1514493.[2] Zhou S et al. Positron Emission Tomography-Computed Tomography Surveillance after (Chemo)Radiotherapy in Advanced Head and Neck Squamous Cell Cancer: Beyond the PET-NECK Protocol. Clinical Oncology 32 (2020) 665e673.