Generating change through collaboration - a clinician-led IGRT framework for head and neck radiotherapy
Purpose/Objective
Image guided radiotherapy (IGRT) in head and neck cancer treatment can be challenging due to complexities presented by variable target and organ at risk (OAR) position. In the authors department an audit of 178 consecutive patients found primary target baseline shifts occurred in 17% of patients (30/178). When baseline shifts are detected by radiographers (RTTs) initial referral online is to departmental IGRT advanced practitioner radiographers (IGRT APRTT). Decision making by IGRT APRTTs can be subjective, introducing a level of uncertainty during the online IGRT process. It also increases the time taken for treatment to take place.
Departmental protocol is to image first three days and then weekly (eNAL). Audit data demonstrated that 54.3% of all head and neck fractions were imaged, a significant increase upon the expected 24% for an eNAL protocol. This imaging workload provided an impetus to consider daily imaging for head and neck treatment. The clinical head and neck team within the authors department acknowledged this and wanted to provide robust protocols that would aid decision making and establish a clinician approved scope of practice for both RTTs and IGRT APRTTs. The aim of this report is to detail the project pathway and evaluate the effectiveness of the developed framework.
Material/Methods
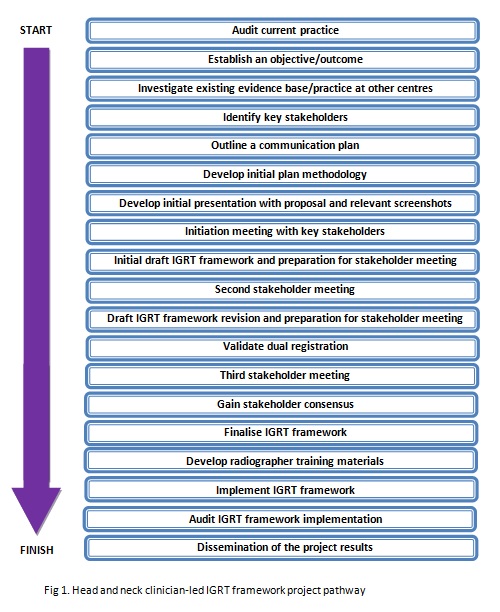
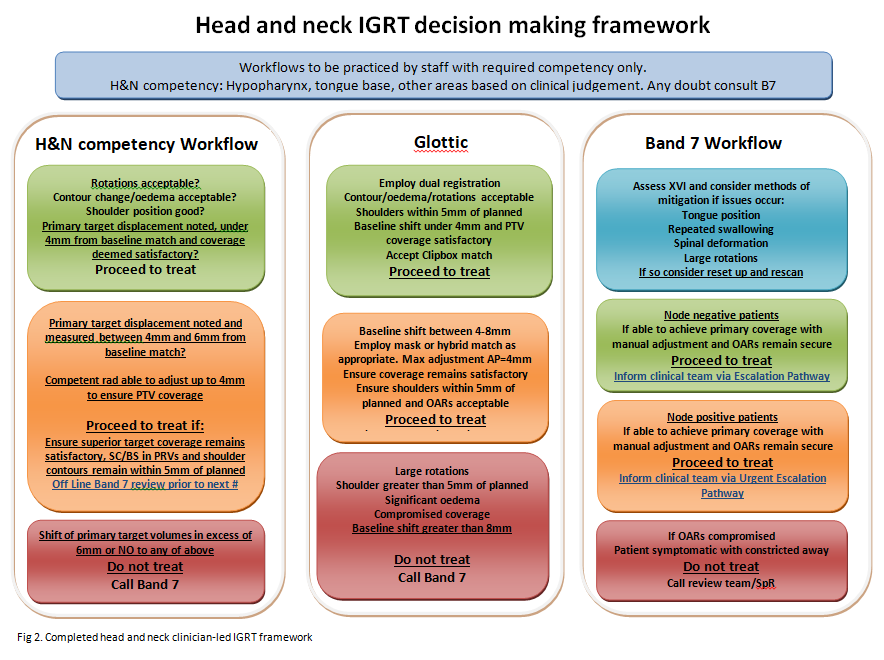
The intent was to apply principles of project management planning and develop the framework within a systematic framework. The project pathway steps are illustrated in figure 1. A timeframe of 6 months was established for completion. Using the 178 patients included within the audit, relevant CBCT images with primary target baseline shifts were reviewed by an interdisciplinary team. The members consisted of the head and neck consultant group (5 clinicians), head of treatment planning, radiotherapy technical lead, pre-treatment RTT, IGRT APRTT team representative, and two RTTS. Images were discussed and consideration for optimising online and offline interventions was made. Based on consensus judgements thematic trends were categorised. A decision making framework was constructed to cover various scenarios with recommended actions dependent on thresholds. Established actions levels were based on severity:
- Green - proceed to treat
- Amber- proceed to treat with required intervention online/offline
- Red - do not treat
Prior to implementation a dual registration methodology for glottis treatments was validated (described in a supporting abstract), training materials were developed and a pilot timing study was carried out to determine if implementation would lead to improvements in efficiency. 20 glottic, hypopharyngeal and tongue base patients were included in the timing study. Two RTTs involved in the development of the project employed the scope of practice outlined by the framework to online image reviews. In order to capture the complete IGRT process timing began at the start of CBCT acquisition and was recorded when the first treatment VMAT arc was initiated. Although no further changes within the department were made that might have influenced IGRT review the timing study included timing for online image review from other RTTs without use of the framework scope of practice. This allowed comparison for scenarios where escalation to IGRT APRTTs was needed and where no escalation was required.
Results
The head and neck IGRT framework (figure 2) project pathway was completed in 146 days and within the projected 6 months (153 days). The process began 18th May 2023 (audit results completed and disseminated/project outcome established) and was finalised 11th October 2023 (dissemination of project results).
20 patients and 60 images were included within the pilot timing study. Images that required no escalation resulted in a mean time of 3:08 minutes calculated as from start of CBCT acquisition until the first treatment VMAT arc was initiated. For image reviews which required escalation to an IGRT APRTT the mean time taken was 7:08 minutes. For a subset of twenty images reviewed by RTTs under the decision making framework, which would have otherwise been escalated to IGRT ARPTTs, the mean image review time was 4:08 minutes. This represents a 42% reduction in image workflow time compared to the department’s standard method of escalation to IGRT ARPTTs.
Conclusion
Employing a collaborative interdisciplinary approach using project management principles in the development of an IGRT decision making framework for head and neck radiotherapy lead to a successful and efficient outcome. It encouraged the establishment of a consensus approach and has allowed scope and opportunity to develop creative solutions in managing primary target displacement, such as the use of dual registration. Furthermore it has augmented and expanded the RTT IGRT scope of practice, helped standardise actions and reduce uncertainty, and improved on-treatment efficiency in preparation for adoption of daily imaging.