Gross Tumour Volume predicts survival in HPV related Oropharyngeal Squamous Cell Carcinoma
Purpose/Objective
To investigate if tumour volume (primary, nodal and combined) predicts recurrence free (RFS) and overall survival (OS) in p16+ oropharyngeal squamous cell carcinoma.
Material/Methods
Study design
We conducted a retrospective analysis of patients with OPSCC treated with curative radiotherapy in SLRON from 2013 - 2021. TNM 8th edition definition of stage was applied.
Participants
Eligible participants had OPSCC and received radiotherapy as definitive, radical treatment. Diagnosis was based on clinical assessment, histological sampling and PET imaging. p16 status was available for all patients. Clinical examination and PET imaging were used to assess response to treatment.
Treatment
Patients received 65-70Gy over 30-35 fractions, delivered using Intensity-Modulated Radiotherapy (IMRT).
Endpoints
Primary endpoints:
-
To investigate if GTVp predict RFS & OS in p16+ OPSCC
-
To investigate if GTVn predict RFS & OS in p16+ OPSCC
-
To investigate if GTVcomb predict RFS & OS in p16+ OPSCC
Secondary endpoints:
-
To investigate if GTVp &/or GTVn predict RFS & OS in p16- OPSCC
-
To investigate if GTVp &/or GTVn predict RFS & OS in OPSCC
-
To investigate if use of concomitant chemotherapy improves outcomes in OPSCC in this cohort
-
To estimate RFS and OS
Statistical Analysis
All analyses were performed in IBM SPSS Statistics ver 29.0, and involved descriptive statistics, survival analyses by Kaplan-Meier method, and linear regression by Cox Proportional Hazards (univariate & multivariate). OS was evaluated from date of final RT. RFS was evaluated from date of final RT to the date of first local or distant recurrence, death, or last clinical assessment/investigation.
Results
Baseline Characteristics
From January 2013 to April 2021, 246 patients were eligible for this review. Median age at first RT was 59.6. 187 (76%) were male. 179 (73%) had p16+ disease. 218 (88.6%) received chemotherapy. Median follow up was 25.5 months (0.5 - 96).
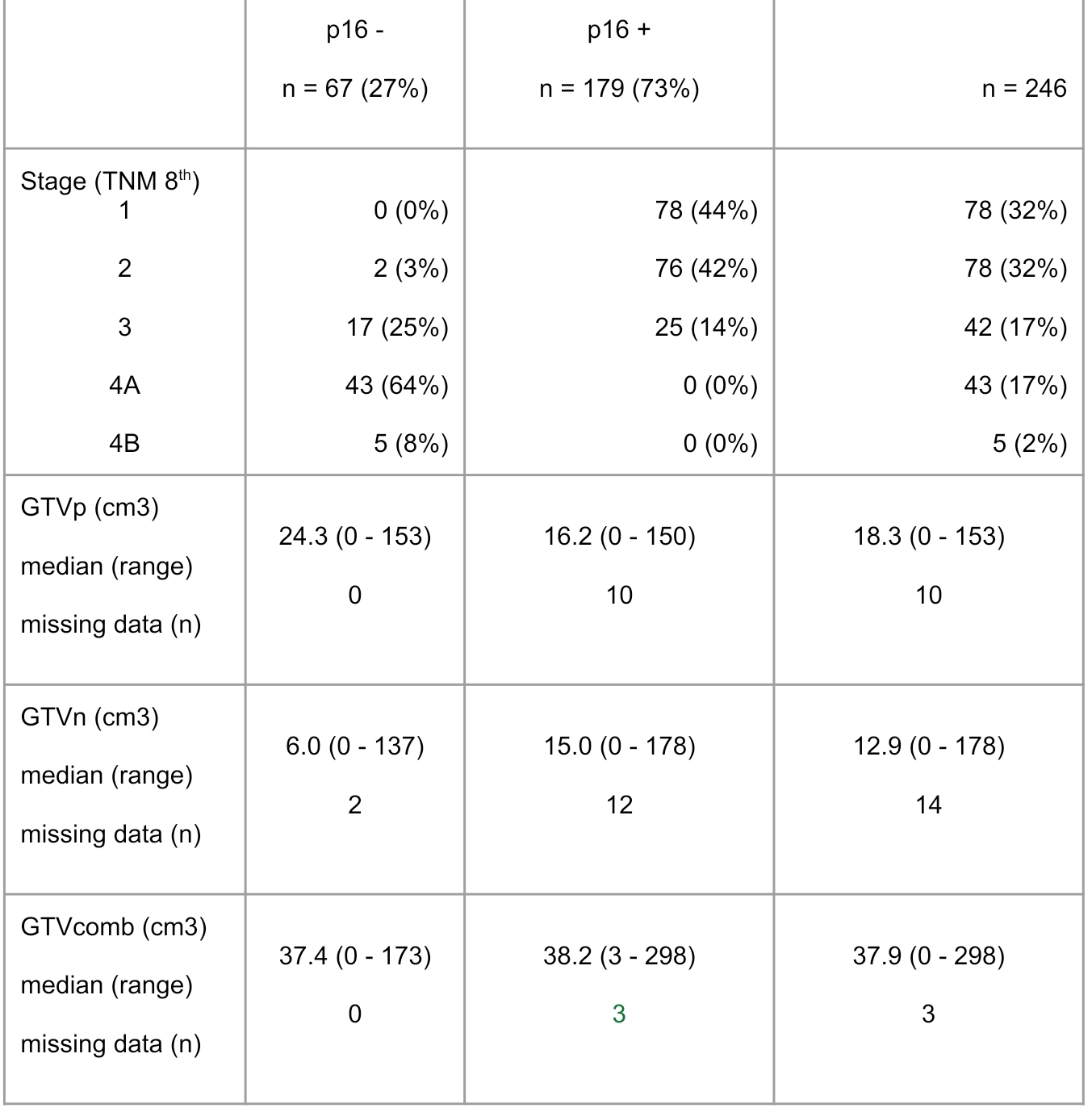
Disease stage & Tumour volumes
Patients with p16+ disease were diagnosed with earlier stage disease (86% stage 1 or 2), in comparison with those with p16- disease (3% stage 3 or 4; p< .001).
Treatment
Treatment was delivered using IMRT. 235 (95.5%) received 70Gy in 35 fractions and 11 (4.5%) received 65Gy in 30 fractions.
Overall Survival
61 out of 246 patients (25%) died. Median survival for the total population was not reached. 3, 4 and 5 year overall survival was 75% (95%CI: 69 to 81%), 69% (95%CI: 61 to 76%) and 64% (95%CI: 55 to 73%) respectively.
There was a significant difference in OS between those with P16- and P16+ (p<.001).
Median survival for the P16- population was 34.9 months (95%CI 13 to 56 months).
Median survival for the P16+ population was not reached.
Recurrence Free Survival
Median recurrence free survival for the total population was not reached.3, 4 and 5 year RFS survival was 65% (95%CI: 59 to 72%), 63% (95%CI: 56 to 70%) and 58% (95%CI: 49 to 66%) respectively.
There was a significant difference in RFS between those with P16- and P16+ (p<.001).
Median survival for the P16- population 23.6 months (95%CI 11 to 37 months).
Median survival for the P16+ population was not reached.
Survival based on Gross Tumour Volume
For the total population (p16+ & p16-):
- GTVp greater or less than median GTVp (dichotomized) was a statistically significant predictor of OS (p= .004)
- GTVp based on Adrian et al volume brackets <6 cm3, 6–12 cm3, 12–24 cm3, 24–48 cm3, 48–96 cm3, and>96cm3 (as suggested by Adrian et al, 2022) was a statistically significant predictor of OS (p<.001)
- GTVp greater or less than 40cm3 (as suggested by Adrian et al, 2022) was a statistically significant predictor of OS (p<.001)
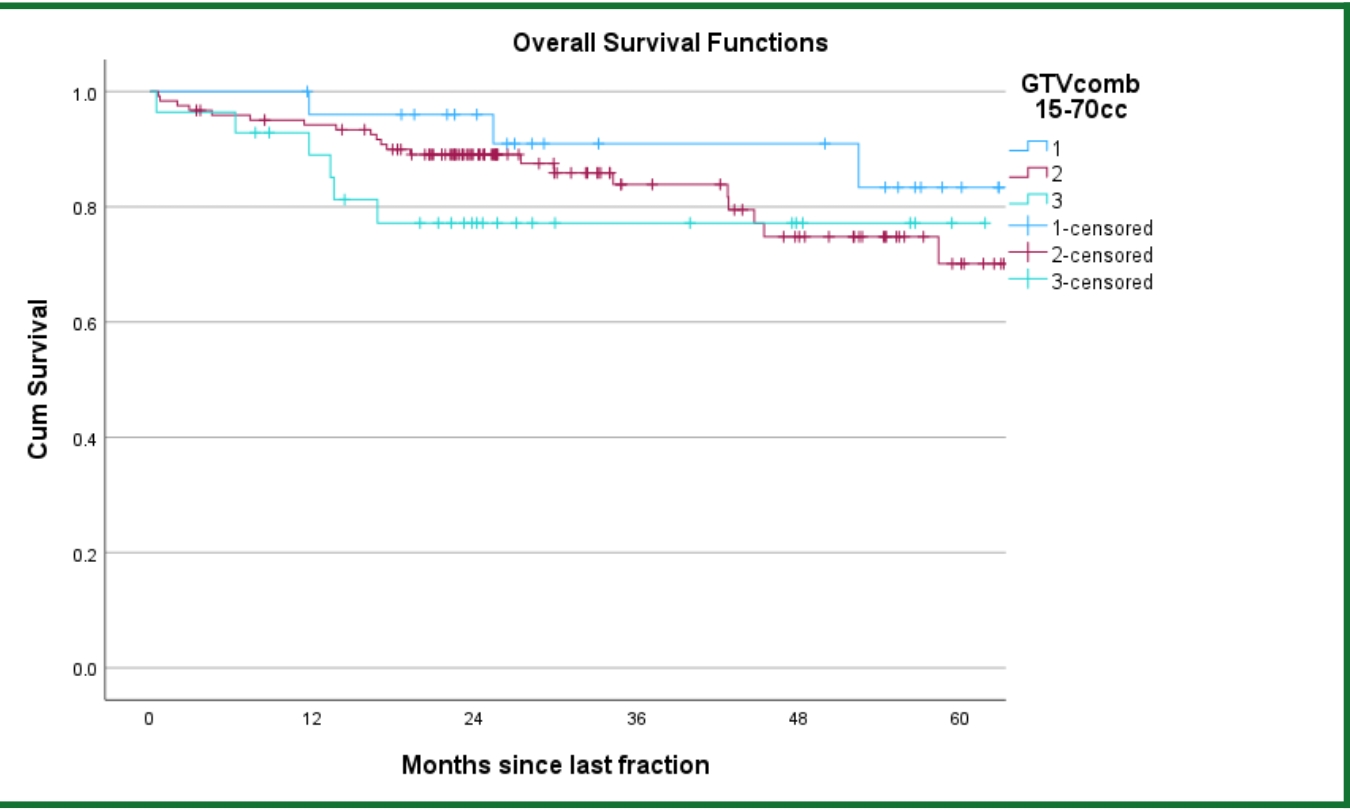
- GTVcomb based on volume brackets <15cc, 15-70cc, >70cc (as suggested by Panje et al, 2017) was a statistically significant predictor of OS and RFS (p= .001 and p<.001 respectively).
When looking only at those with P16+, neither age, gender nor stage 1-2, were predictive of OS. The following variables were predictive of OS: GTVp, GTVp >18.3cc, GTV as per Adrian et al volume brackets, GTVp 15-70cc, GTVp>40cc, GTVn, GTVcomb and total dose.
Conclusion
We demonstrate that GTV (primary, nodal and combined) predict outcome in p16+ OPSCC. This metric is readily available to the Radiation Oncologist at tumour delineation, and therefore may aid dose de-escalation decision making, without added delay.
Future work may investigate cautious dose de-escalation in a cohort with smaller GTVs.
1. Fakhry C. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. Journal of the National Cancer Institute : JNCI. 2008;100(4):261–9.2. Masterson, L., et al. "De-Escalation Treatment Protocols for Human Papillomavirus-Associated Oropharyngeal Squamous Cell Carcinoma: A Systematic Review and Meta-Analysis of Current Clinical Trials." European Journal of Cancer, vol. 50, no. 15, 2014, pp. 2636-2648.3. Adrian, G., Carlsson, H., Kjellén, E. et al. Primary tumor volume and prognosis for patients with p16-positive and p16-negative oropharyngeal squamous cell carcinoma treated with radiation therapy. Radiat Oncol 17, 107 (2022). 4. Gabani, P., et al. "Radiation Therapy Dose De-Escalation Compared to Standard Dose Radiation Therapy in Definitive Treatment of HPV-Positive Oropharyngeal Squamous Cell Carcinoma." Radiotherapy and Oncology, vol. 134, 2019, pp. 81-88.5. Lee, N., et al. "Strategy of using Intratreatment Hypoxia Imaging to Selectively and Safely Guide Radiation Dose De-Escalation Concurrent with Chemotherapy for Locoregionally Advanced Human Papillomavirus–Related Oropharyngeal Carcinoma." International Journal of Radiation Oncology Biology Physics, vol. 96, no. 1, 2016, pp. 9-17.6. Swisher-McClure, S., et al. "A Phase 2 Trial of Alternative Volumes of Oropharyngeal Irradiation for De-Intensification (AVOID): Omission of the Resected Primary Tumor Bed After Transoral Robotic Surgery for Human Papilloma Virus–Related Squamous Cell Carcinoma of the Oropharynx." International Journal of Radiation Oncology Biology Physics, vol. 106, no. 4, 2020, pp. 725-732.