Head and Neck Re-Irradiation: Toxicity Analysis and Correlation between Toxicity and Dosimetric Parametres
Purpose/Objective
As radiotherapy (RT) is fundamental for definitive treatment of head and neck carcinomas and novel modulated techniques permit more selected patients to be re-irradiated, we aimed to collect data about chronic and acute toxicity after second irradiation and evaluate correlation with dosimetric parameters, for future specification of organ at risk constraints.
Material/Methods
Retrospective analysis of 60 patients treated at our institution for loco-regional relapse or second primary head and neck tumor, re-irradiated between 2009 and 2023 to a previously irradiated location (>50Gy) using 3D or IMRT with a total dose of 60Gy (mean 60Gy, range 54-70Gy) at 2-2.1Gy/Fx. Data about acute and chronic toxicity was collected from clinical reports, according to CTCAEv5.
We were able to evaluate dosimetric data about 59 patients. For data extraction, rigid registration was made with TPS Eclipse. Sum plan of both treatments was created (dose distribution were not converted to EQD2 because of TPS limitations) on the most recent CT scan. Dosimetric data were extracted using homemade script from API Eclipse. Planning and calculation system: Eclipse (v10-v15.6). Calculation algorithm: AAA for IMRT plans, Acuros XB for VMAT plans.
Results
Acute toxicity after re-irradiation was very common (95%). 70% presented mucositis (28 out of 32 were G1-2) and 67% epithelitis (35 out of 40 were G1-2). Chronic toxicity after second RT consisted of dysphagia (74,5% of the patients, with 23 patients requiring use of nasogastric tube (NGT) or Percutaneous Endoscopic Gastrostomy (PEG), of which 16 were attributed to RT toxicity and not to prior treatment sequelae), osteonecrosis (6 patients), fistula (5 patients), trismus (24% G1-2, 3.3% G3-4). Carotid rupture happened in one patient.
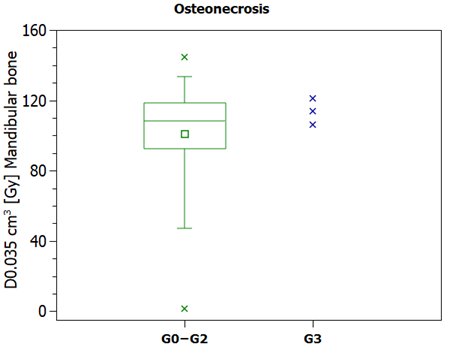
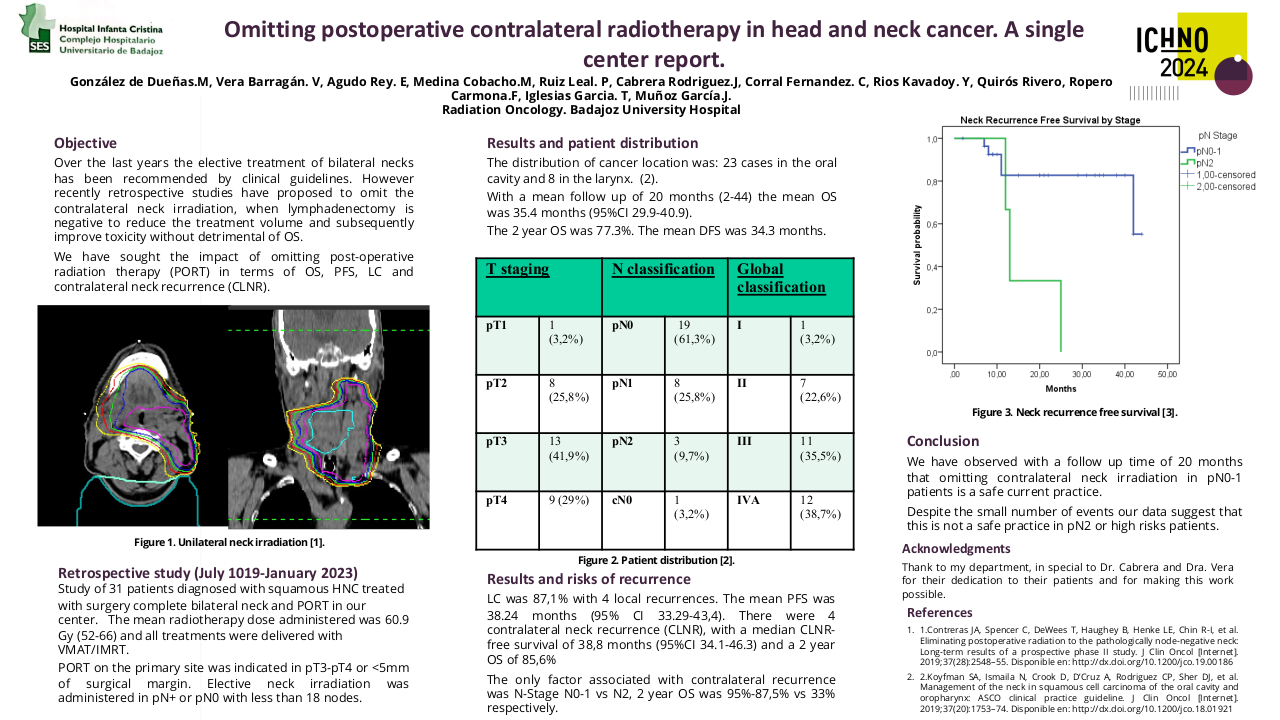
Of 6 patients presenting osteonecrosis, 3 were grade 3, with no patients with grade 4 toxicity. Looking at the plan sum, these all three patients had received a total D0.035 > 100Gy to the mandible bone, and received a higher mean dose (113.7Gy vs 100.8Gy) to the mandible compared with patients who presented milder or no toxicity (Figure 1).
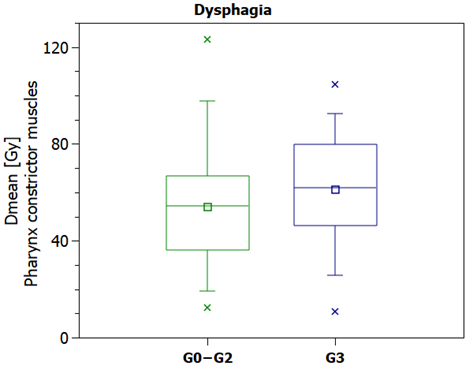
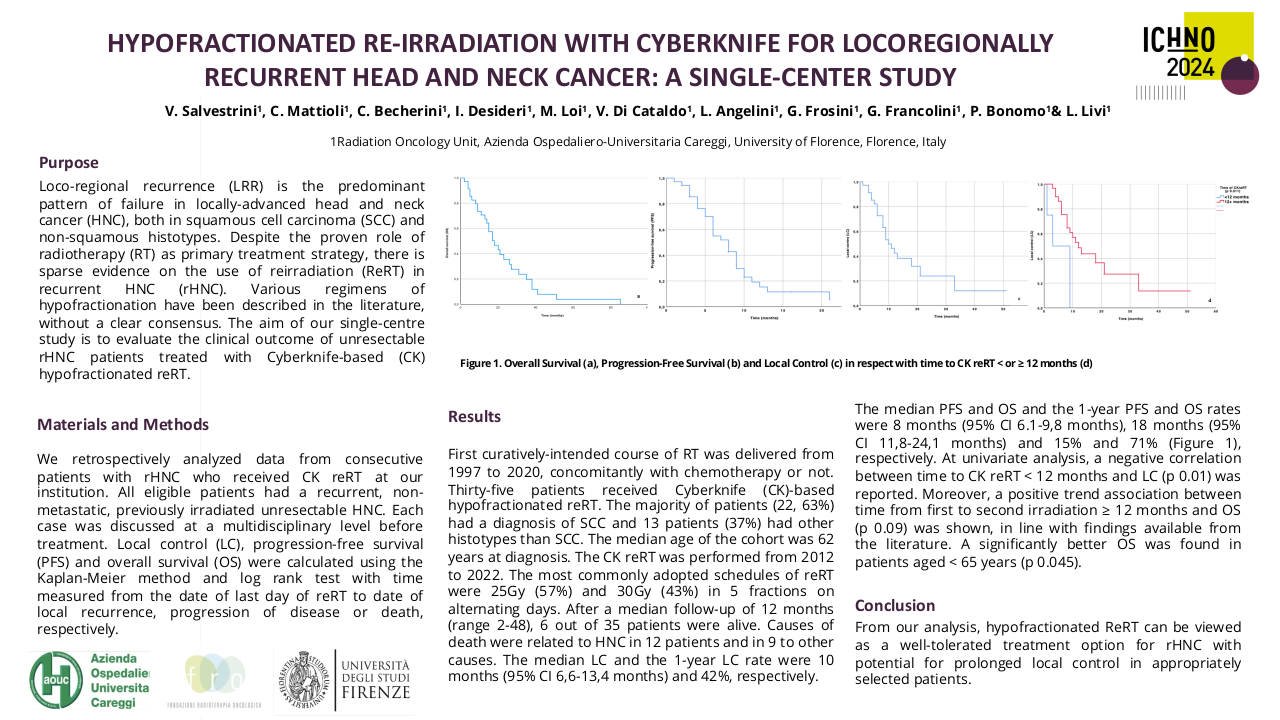
For dysphagia, we analysed mean dose to pharynx constrictor muscles. We can see that those needing PEG/NGT (G3 toxicity) receive a higher mean dose (61Gy vs 53Gy) than those who don't need it. Of the 16 patients who required these interventions due to RT toxicity (not because of surgery sequelae or similar), the received dose is still higher (60.4Gy) than the mean dose received in patients without PEG or NGT (Figure 2).
Univariate model showed that those who required NGT or PEG after re-irradiation because of RT toxicity present higher risk of events, with HR of 3.05 (1.57-5.92, p<0.001). No statistically significant differences were seen for treatment technique (IMRT vs 3D) or other variables, also for the multivariable analysis.
Figure 1. Osteonecrosis according to toxicity grade (G0,1,2 vs G3). D0.035cm3 summation (First RT treatment and re-RT) in Gy to the mandibular bone.
Figure 2. Dysphagia according to toxicity grade (G0,1,2 vs G3). Dmean summation (First RT treatment and re-RT) in Gy to the pharynx constrictor muscles.
Conclusion
Toxicity after re-irradiation in head and neck càncer patients is not negligible. Despite acute effects are the most frequent ones, regarding long term toxicity, dysphagia is the most frequent and the one with more impact in the quality of life of the patient, but this, as well as the other toxicities are rare to have a severe presentation (G3 or more). Our data seems to show a correlation between dose to the mandible bone and G3 osteonecrosis, but interpretation must be cautious, as the limitations of this analysis include the rigid dose registration instead of deformable, no EQD2 dose summation and the relevance of anatomic variations due to surgeries and tumor growth. Further investigations regarding these issues could help to improve the management of re-irradiation dosimetry evaluation.
1. Andratschke et al. European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus on re-irradiation: definition, reporting, and clinical decision making. Lancet Oncol 2022; 23: e469–78.2. Vargo JA, Moiseenko V, Grimm J, et al. Head and Neck Tumor Control Probability: Radiation Dose-Volume Effects in Stereotactic Body Radiation Therapy for Locally Recurrent Previously-Irradiated Head and Neck Cancer: Report of the AAPM Working Group. Int J Radiat Oncol Biol Phys. 2021;110(1):137-146. doi:10.1016/j.ijrobp.2018.01.0443. Ward et al. Retreatment of Recurrent or Second Primary Head and Neck Cancer After Prior Radiation: Executive Summary of the American Radium Society (ARS) Appropriate Use Criteria (AUC). Int J Radiat Oncol Biol Phys 2022; 15, 113 (4): 759-786.