The prognostic value of tumour p16 status in non-oropharyngeal head and neck squamous cell carcinoma.
Purpose/Objective
Compared to oropharyngeal squamous cell carcinoma (SCC), the association between p16 status and outcome in non-oropharyngeal head and neck squamous cell carcinoma (HNSCC) is less clear. We conducted this single-institutional study to evaluate the prognostic value of p16 status in this population.
Material/Methods
A retrospective review was conducted for all newly diagnosed non-metastatic HNSCC arising from larynx, hypopharynx, sinonasal mucosa, and oral cavity tested for p16 and treated with curative intent between Jan 2009 and December 2021 in our institution. p16 immunohistochemistry (IHC) staining was routinely performed in laryngeal and hypopharyngeal cancer during 2014 and 2017 for EORTC1219 trial eligibility, and for selected non-oropharyngeal HNSCC if the patients were non-smokers/non-drinkers, or if tumours were non-keratinizing or of basaloid morphology. All p16 IHC was performed and interpreted at our institution by experienced head and neck pathologists. p16 positivity was defined by diffuse cytoplasmic and nuclear staining in >70% tumour cells. A proportion of tumours was also tested for HPV DNA by polymerase chain reaction (PCR). Overall survival (OS), disease-free survival (DFS), locoregional control (LRC) and distant control (DC) were compared between p16-positive and p16-negative cohorts. Multivariable analysis was performed to evaluate the prognostic value of tumour p16 status on OS.
Results
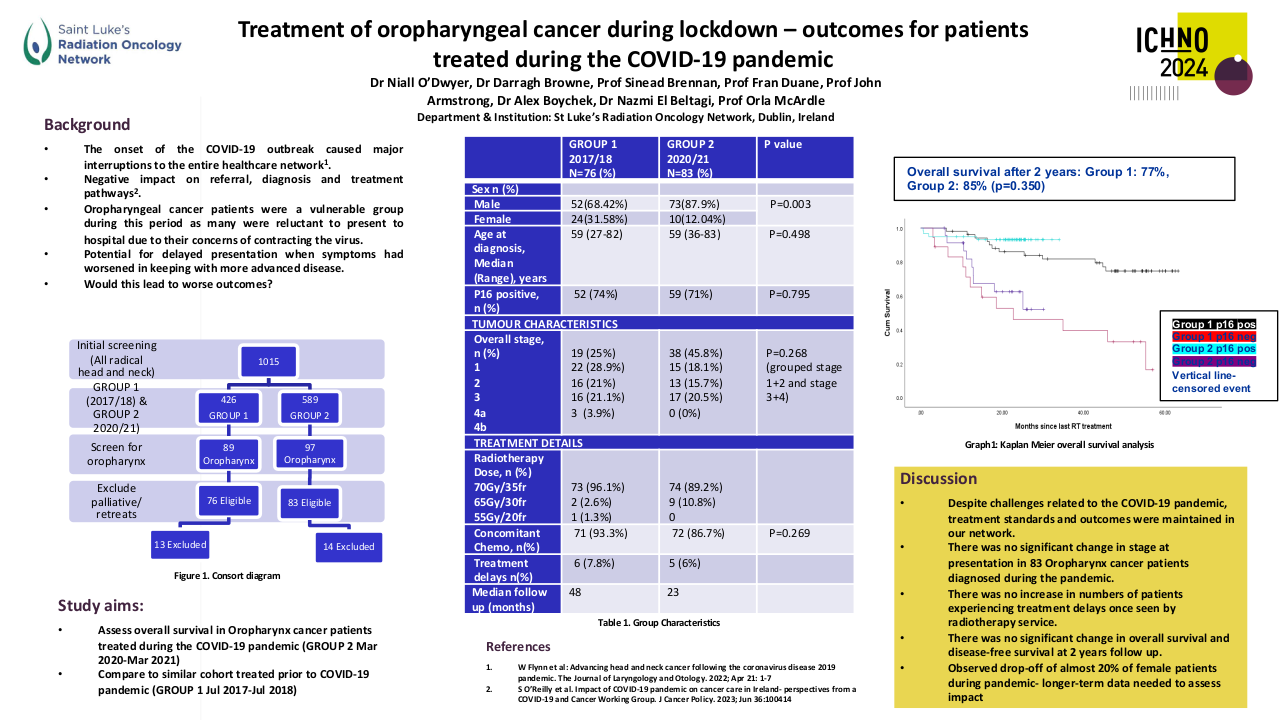
Of 3176 consecutive non-oropharyngeal HNSCC, p16 was tested in 466 (15%) patients, of whom 91 (20%) were p16-positive (26 larynx, 20 hypopharynx, 35 sinonasal tract, and 10 oral cavity) and 375 (80%) were p16-negative (162 larynx, 67 hypopharynx, 31 sinonasal tract, and 115 oral cavity). PCR for HPV DNA was performed in 39 p16-positive and 28 p16-negative cases and revealed 100% concordance between p16 IHC and HPV DNA. The most common HPV genotypes were single infection HPV-16 (69.2%), single infection HPV-18 (10.3%), co-infection HPV 16 & 18 (2.6%), co-infection HPV 16 & 51 (2.6%) and other HPV genotypes (15.4%). The median age of patients tested was 62.5 years (range 54.5-70.5). Patients with p16-positive tumour had lower smoking pack-years compared to patients with p16-negative tumour (median 12.5 vs 30, p<0.001). There was no difference in TNM-8 T-category (p=0.09) and N-category (p=0.20) distribution between the two cohorts. Sinonasal primary site had the highest p16-positive rate (35/66, 53%), followed by hypopharynx (20/87, 23%), larynx (26/188, 14%), and oral cavity (10/125, 8%). Median follow up was 4.6 years (range 0.2-13.2). p16-positive non-oropharyngeal HNSCC had higher 5-year OS (80% vs 58%, p<0.001), DFS (73% vs 48%, p<0.001), LRC (89% vs 75%, p=0.003), and DC (91% vs 80%, p=0.007) vs p16-negative. Multivariable analysis, adjusting for primary disease site, age, smoking history, TNM-8 T-categories, N-categories, and use of systemic therapy, confirmed the prognostic importance of p16-positivity on OS (adjusted hazard ratio 0.46, 95% confidence interval 0.28 to 0.75, p=0.002). Sub-site analysis revealed p16-positive laryngeal and hypopharyngeal SCCs had higher 5-year OS (larynx: 89% vs 63%, p=0.015; hypopharynx: 77% vs 35%, p=0.003); and DFS (larynx: 85% vs 52%, p=0.004; hypopharynx: 67% vs 24%, p<0.001) vs p-16 negative counterparts. A non-significant trend toward better 5-year OS (82% vs 42%, p=0.051) and DFS (75% vs 42%, p=0.054) were observed in p16-positive sinonasal SCCs. However, no difference in OS (57% vs 66%, p=0.852) and DFS (50% vs 56%, p=0.906) was observed in p16-positive versus p16-negative oral cavity SCC (Table 1).
Table 1. Outcomes by p16 Status in Non-Oropharyngeal Squamous Cell Carcinoma
|
5-year Outcomes |
|
Case No |
OS |
DFS |
LRC |
DC |
|
Total |
HPV+ |
91 |
80% |
73.0% |
89% |
91.0% |
|
n=466 |
HPV(-) |
375 |
58% |
48.0% |
75% |
80.0% |
|
|
p value |
|
<0.001 |
<0.001 |
0.003 |
0.007 |
|
Larynx |
HPV+ |
26 |
89% |
85.0% |
100% |
92% |
|
n=188 |
HPV(-) |
162 |
63% |
52.0% |
79% |
82% |
|
|
p value |
|
0.015 |
0.004 |
0.015 |
0.195 |
|
Hypoph |
HPV+ |
20 |
77% |
67.0% |
83% |
78% |
|
n=87 |
HPV(-) |
67 |
35% |
24.0% |
68% |
66% |
|
|
p value |
|
0.003 |
<0.001 |
0.117 |
0.12 |
|
Sinonasal |
HPV+ |
35 |
82% |
75.0% |
84% |
97% |
|
n=66 |
HPV(-) |
31 |
42% |
42.0% |
63% |
88% |
|
|
p value |
|
0.051 |
0.054 |
0.053 |
0.227 |
|
OSCC |
HPV+ |
10 |
57% |
50.0% |
90% |
100.0% |
|
n=125 |
HPV(-) |
115 |
66% |
56.0% |
76% |
85.0% |
|
|
p value |
|
0.852 |
0.906 |
0.302 |
0.193 |
Conclusion
In this selected cohort of non-oropharyngeal HNSCC, p16-positive status carries a survival advantage (HR 0.46) which is similar to the 0.49 HR of HPV-positive status reported in RTOG 0129 (Ang et al. 2010) for oropharyngeal carcinoma. This 5-year OS difference is mainly seen in laryngeal (26% absolute OS difference) and hypopharyngeal (42% absolute OS difference) SCC, possibly in sinonasal SCCs, but not in oral cavity SCC. The association of p16 and HPV, as well as its prognostic value should be confirmed in large systematically tested datasets.
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, Westra WH, Chung CH, Jordan RC, Lu C, Kim H, Axelrod R, Silverman CC, Redmond KP, Gillison ML. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010 Jul 1;363(1):24-35. doi: 10.1056/NEJMoa0912217.