How applicable are the results of the DARS trial to current practice? A comparison of average dose to the pharyngeal constrictor muscles.
Purpose/Objective
The DARS trial is a phase 3, multicentre, randomised controlled trial published by Nutting et al in 2023 (1). Within the trial, patients with oropharyngeal or hypopharyngeal cancer were randomised to dysphagia optimised intensity-modulated radiotherapy (DO-IMRT) or standard IMRT. The trial demonstrated that patients in the DO-IMRT group had significantly higher MD Anderson Dysphagia Inventory (MDADI) composite scores at 12 months than patients in the standard IMRT group.
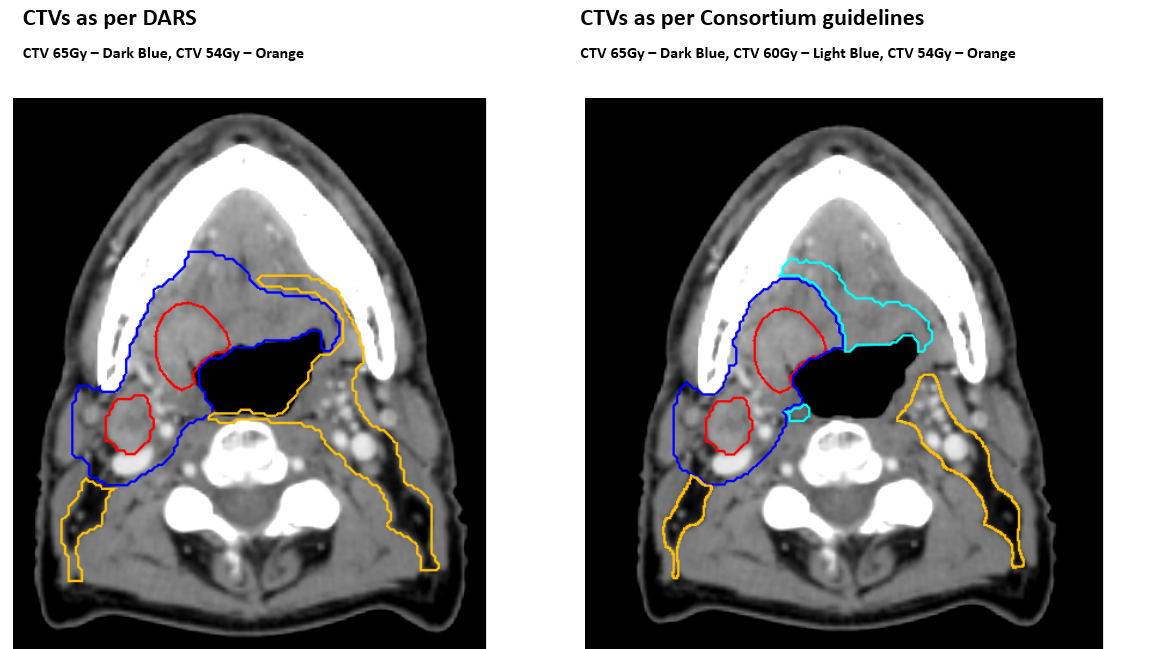
The DARS protocol for the delineation of the primary tumour clinical target volumes (CTVp) included an anatomical approach. A 10 mm margin was added to the Gross tumour volume (GTV) to construct a high-dose clinical target volume, which was to receive 65Gy in 30 fractions. The remaining primary tumour subsite was then delineated to form a low dose CTV to receive 54Gy in 30 fractions (2).
In 2017 the consensus guidelines on delineation of the primary tumour CTV were published by Gregoire et al (3). These guidelines recommend two CTVs for the primary tumour. A 5mm margin is added to the GTV to construct the high-dose CTV, and an additional 5mm rim of tissue is added to form the lower dose CTV. Our centre has adopted these guidelines, and their use is recommended in RCR consensus statements. (4)
Given the differences in the delineation of the high and low dose CTVs between consensus guidelines and the approach used in the DARS trial, one could question how applicable the results of the DARS trial are to wider practice as doses to OARs are likely to be different.
We aimed to assess the validity of the DARS trial findings by comparing average mean dose to the pharyngeal constrictor muscles when CTVs were delineated according to the consensus guidelines (3) and compare these to the standard IMRT and DO-IMRT groups within the DARS trial (2).
Material/Methods
Patients treated at our institution between March 2020 and March 2023 were screened for eligibility, mirroring the criteria used in the DARS trial. Patients had to have been treated for oropharyngeal or hypopharyngeal cancer, with radical radiotherapy and bilateral neck treatment. Patients with a primary tumour involving the posterior pharyngeal wall or the post cricoid oesophagus were excluded. Patients had their primary contoured with a 5+5 expansion, as per the consensus guidelines (3) and received 3 dose levels. The high dose CTV received 65Gy in 30 fractions, as per DARS, but the lower dose CTV around the primary received 60Gy in 30 fractions. The nodal high dose CTV was between 5 and 10mm around the nodal GTV and received 65Gy in 30 fractions. The elective lymph node CTV received 54Gy in 30 fractions. PTV margins were 3-5mm. The IMRT treatment was planned using Pinnacle, using 2 full VMAT arcs.
The pharyngeal constrictor muscles were delineated on the CT planning scans, either by a radiation oncologist, or by the LIMBUS AI outlining software and edited appropriately. As per the DARS protocol, the superior and middle pharyngeal constrictor muscles (SMPCM) were defined as a single structure with the inferior pharyngeal constrictor muscle (IPCM) defined separately. No dose constraints had been applied to the constrictors when planning, and PTV coverage had not been compromised for them. The mean dose to each structure, not overlapping with CTV65Gy or CTV60Gy, (Plan_SMPCM and Plan_IPCM) was calculated.
Results
22 eligible patients were identified. 3 (14%) were female and 19 (86%) were male with a median age of 59. 21 patients (95%) had P16 positive oropharyngeal SCC and 1 patient (5%) had hypopharyngeal SCC.
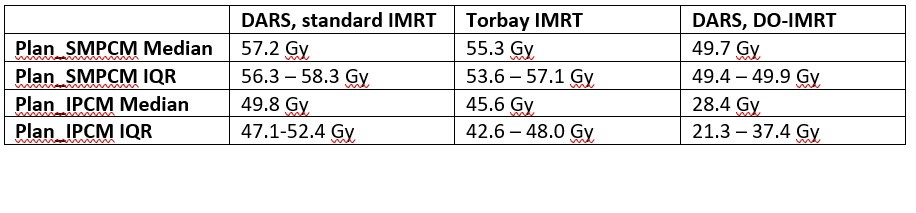
In our cohort, the median of the mean dose to the Plan_SMPCM was 55.3Gy (IQR 53.6-57.1). The median of the mean dose to the Plan_IPCM was 45.6Gy (IQR 42.6-48.0). (See table for comparison)
Conclusion
The average dose to the pharyngeal constructor muscles in our cohort was lower than in the standard arm of DARS, likely reflecting the difference in high and low dose CTV volumes. The average dose, particularly to the IPCM, was significantly higher in our patient group, than in the DARS cohort planned with DO-IMRT. These data support the observation in the DARS trial that DO_IMRT is associated with significantly lower radiation doses to the pharyngeal constrictor muscles, even when accounting for differences in target volume delineation. 83% of patients in the DARs trial had HPV positive OPC, and we conclude DO_IMRT should be considered a standard of care in these good prognosis patients.
1. Nutting C, Finneran L, Roe J, Sydenham MA, Beasley M, Bhide S, Boon C, Cook A, De Winton E, Emson M, Foran B, Frogley R, Petkar I, Pettit L, Rooney K, Roques T, Srinivasan D, Tyler J, Hall E; DARS Trialist Group. Dysphagia-optimised intensity-modulated radiotherapy versus standard intensity-modulated radiotherapy in patients with head and neck cancer (DARS): a phase 3, multicentre, randomised, controlled trial. Lancet Oncol. 2023 Aug;24(8):868-880.2. Petkar I, Rooney K, Roe JW, et al. DARS: a phase III randomised multicentre study of dysphagia-optimised intensity-modulated radiotherapy (DO-IMRT) versus standard intensity-modulated radiotherapy (S-IMRT) in head and neck cancer. BMC Cancer 2016; 16: 770. 3. Gregoire V, Evans M, Le Q et al. Delineation of the primary tumour Clinical Target Volumes (CTV-P) in laryngeal, hypopharyngeal, oropharyngeal and oral cavity squamous cell carcinoma: AIRO, CACA, DAHANCA, EORTC, GEORCC, GORTEC, HKNPCSG, HNCIG, IAG-KHT, LPRHHT, NCIC CTG, NCRI, NRG Oncology, PHNS, SBRT, SOMERA, SRO, SSHNO, TROG consensus guidelines. 4. Radiotherapy and Oncology 2017.10.016. Head and neck cancer: RCR consensus statements. Royal College of Radiologists, 2022.