Survival Analysis of Localized Subglottic Squamous Cell Carcinoma: Therapeutic Options and Outcomes
Purpose/Objective
Primary subglottic Squamous Cell Carcinoma (SCC) is a rare malignancy that accounts for only 1–3% of all laryngeal carcinomas. The selection of therapeutic approaches depends on disease stage and clinical presentation. There are multiple therapeutic options for SCC, including chemotherapy (CTX) and adjuvant radiotherapy (ART). Owing to its rarity, there is no consensus on the best option for improving survival rates. We aimed to explore survival outcomes in terms of overall survival (OS) and cancer-specific survival (CSS) among patients diagnosed with localized SCC who underwent various treatment modalities.
Material/Methods
Data from 2000 to 2019 were obtained from the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) database. Patients who met any of the following criteria were excluded: diagnosis not confirmed by histology, not first tumor or other malignancies in the body, not localized stage or metastasis, and unknown data. Chi-square tests were used to compare clinicopathological features, while survival rates and prognostic factors were identified using the Kaplan-Meier estimator, log-rank tests, and Cox proportional hazard regression.
Results
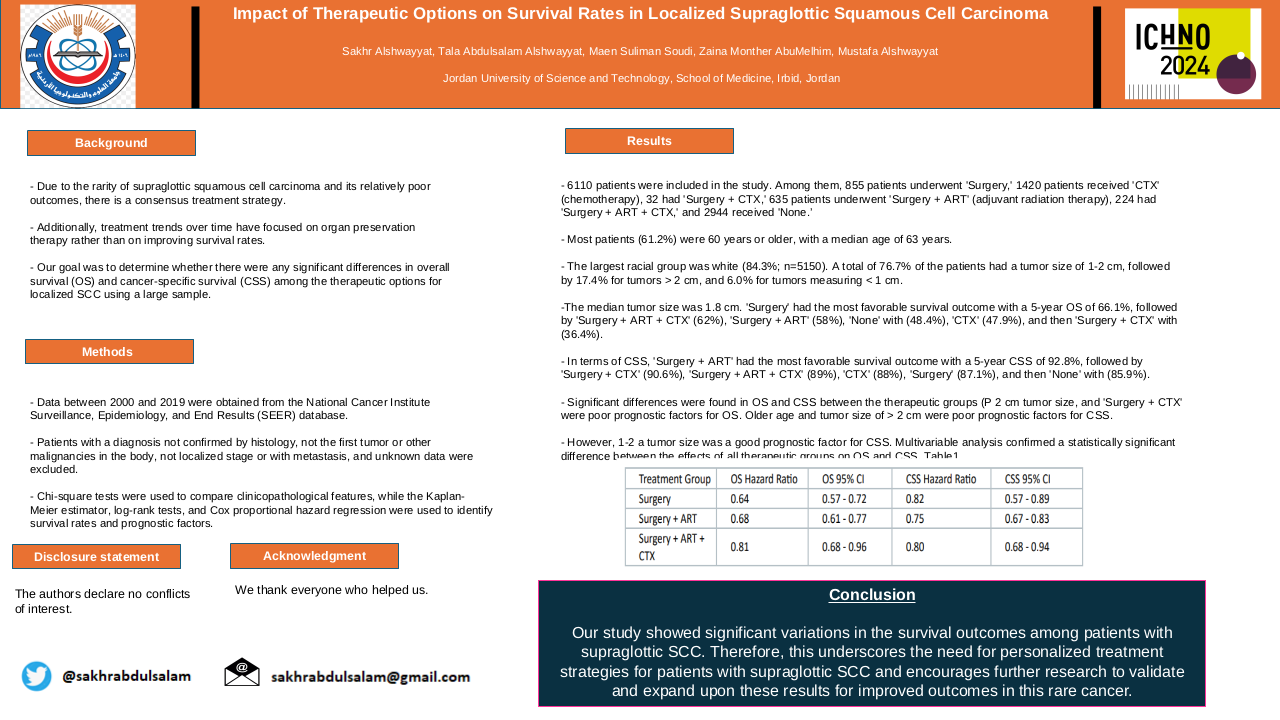
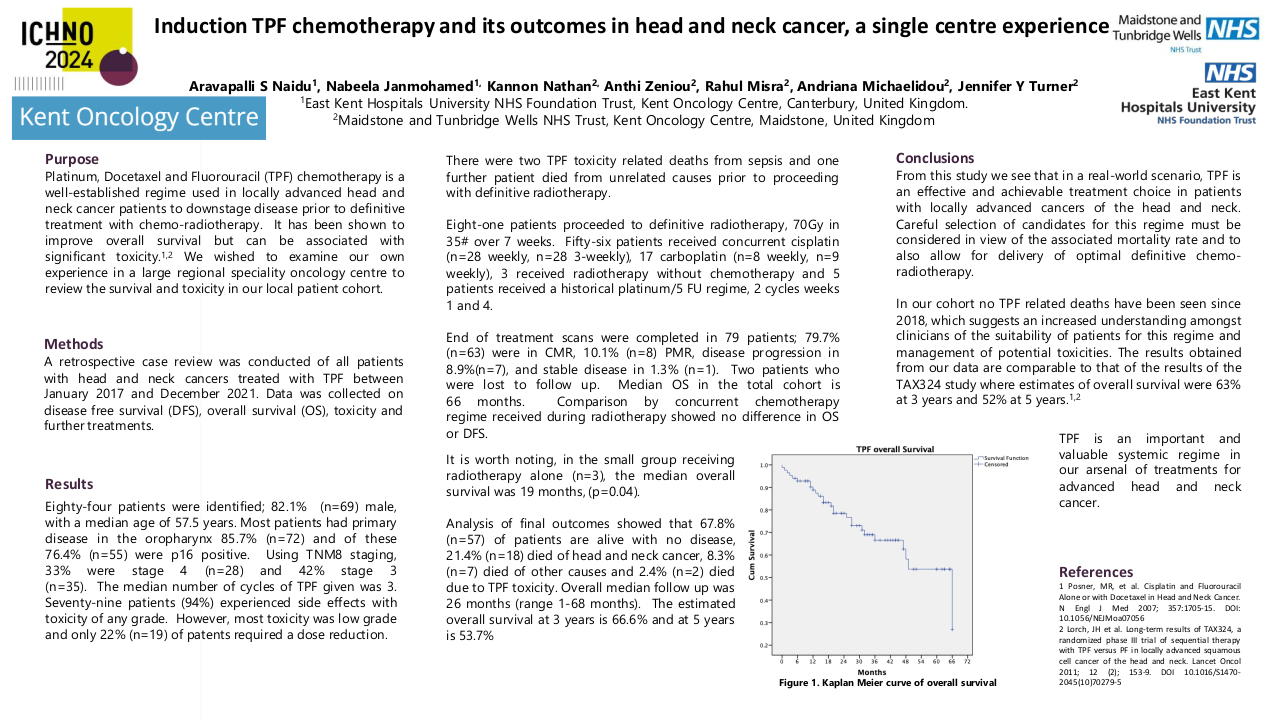
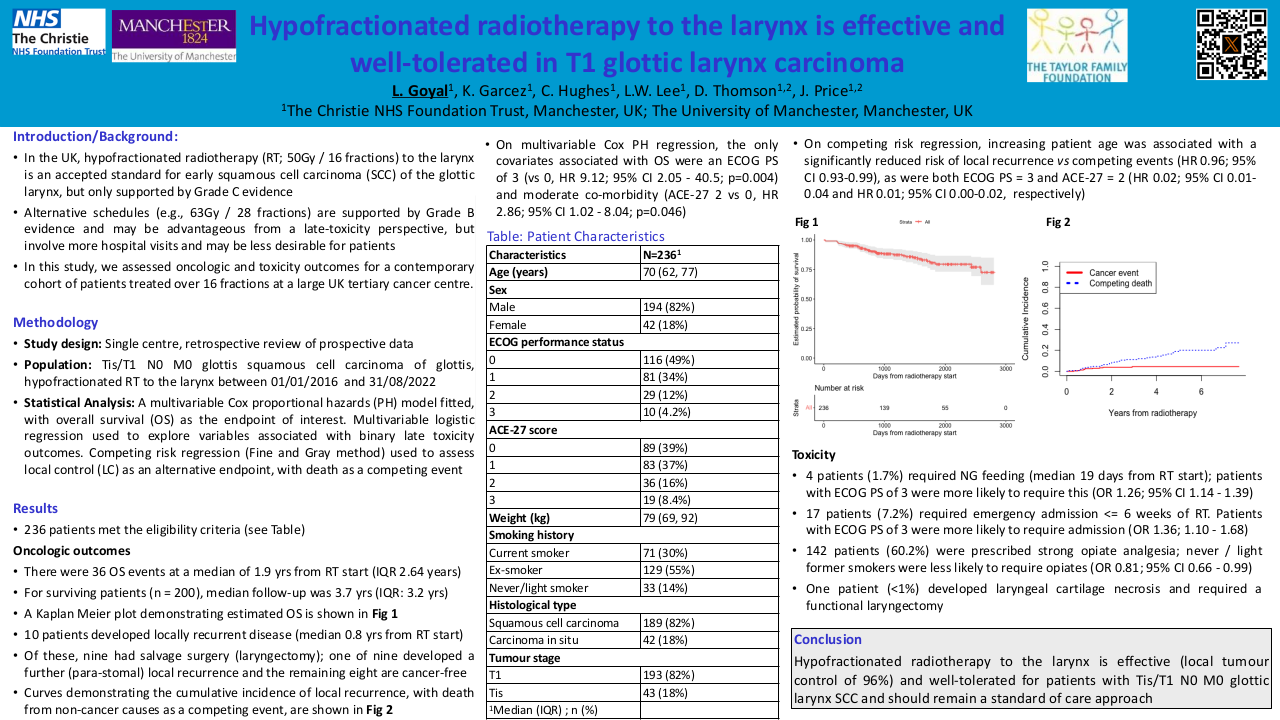
The study population comprised 476 patients. Among them 70 patients with “Surgery,” 101 patients with “CTX,” 89 patients with “Surgery + ART”, 22 with “Surgery + ART + CTX” and 194 “None.” Most patients (68.9%) were 60 years or older, with a median age of 62 years. The largest racial group was white (82.6%; n=328). A total of 79% of the patients had a tumor size greater than 2 cm, followed by 14.1% for 1-2 cm and 6.9% for less than 1 cm. The median tumor size was 2 cm. “Surgery + ART” had the most favorable survival outcome with a 5-year OS of 67.2%, followed by “Surgery” (54.5%), “Surgery + ART + CTX” (93%), “CTX” (51.2%) and then “None” with (46.4%). In terms of CSS, “Surgery + ART” had the most favorable survival outcome with a 5-year CSS of 55.5%, followed by “Surgery + ART + CTX” (55.4%), “CTX” (55.4%) and then “None” with (51.9%) and then “Surgery” (44.3%). Significant differences were found in OS but not CSS between the groups (P<0.0003 and P<0.56, respectively). Older age was a poor prognostic factor for the OS and CSS. White race was a good prognostic factor in OS only. Multivariable analysis confirmed that there is statistically significant difference between the effect of all therapeutic groups on OS, “Surgery + ART” (HR=0.46, 95%CI:0.3-0.7). However, there was no statistical difference in CSS (HR=0.8, 95%CI:0.57-1.4).
Conclusion
The results of this study showed that “Surgery + ART” had the most favorable effect on OS and CSS in SCC patients. Multicenter, prospective studies are required to validate and build upon these findings. However, our results provide a starting point for better understanding of these rare cancers.