Impact of Therapeutic Options on Survival Rates in Localized Supraglottic Squamous Cell Carcinoma
Purpose/Objective
Due to the rarity of supraglottic squamous cell carcinoma and its relatively poor outcomes, there is a consensus treatment strategy. Additionally, treatment trends over time have focused on organ-preservation therapy rather than on improving survival rates. Our goal was to determine whether there were any significant differences in overall survival (OS) and cancer-specific survival (CSS) among the therapeutic options for localized SCC using a large sample.
Material/Methods
Data between 2000 and 2019 were obtained from the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) database. Patients with a diagnosis not confirmed by histology, not the first tumor or other malignancies in the body, not localized stage or with metastasis, and unknown data were excluded. Chi-square tests were used to compare clinicopathological features, while the Kaplan-Meier estimator, log-rank tests, and Cox proportional hazard regression were used to identify survival rates and prognostic factors.
Results
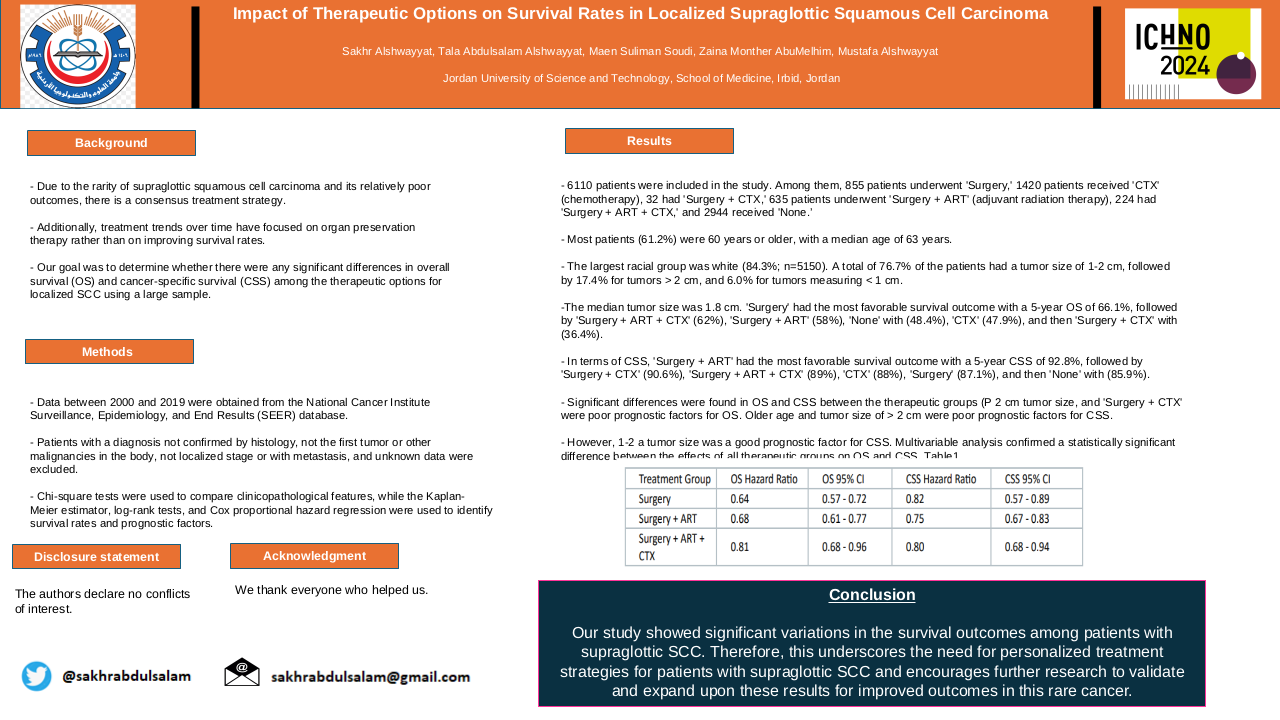
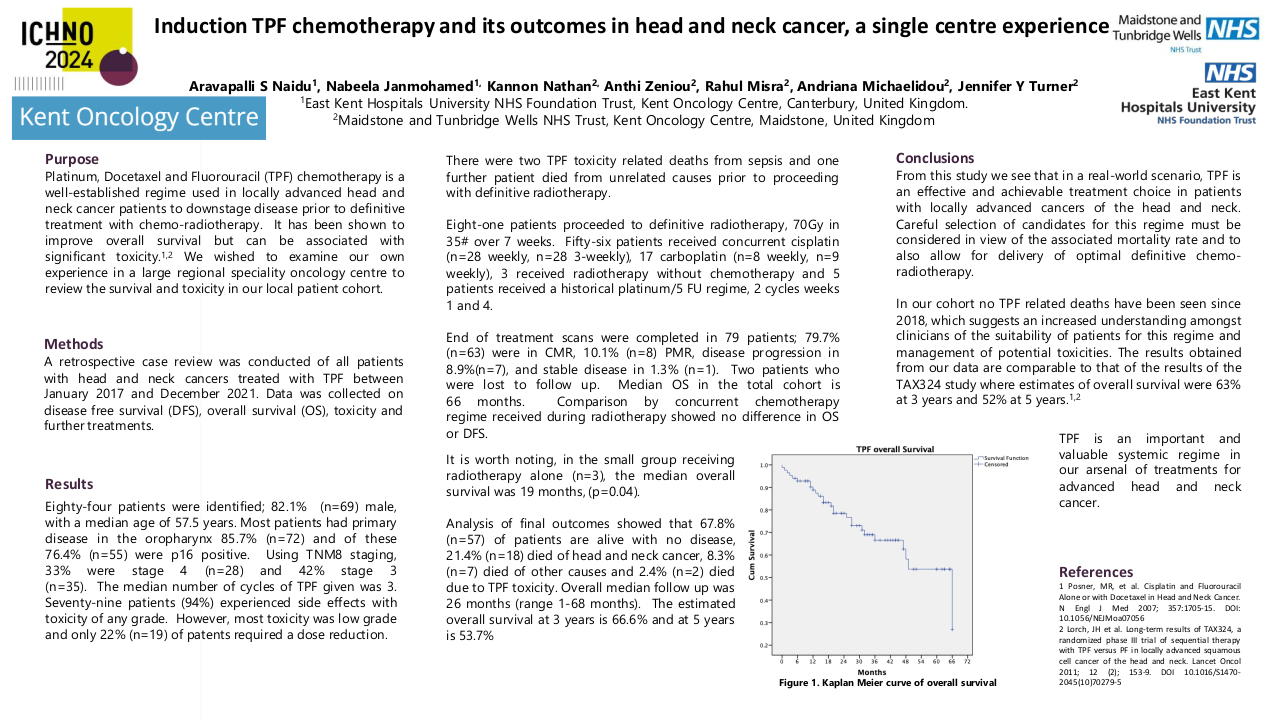
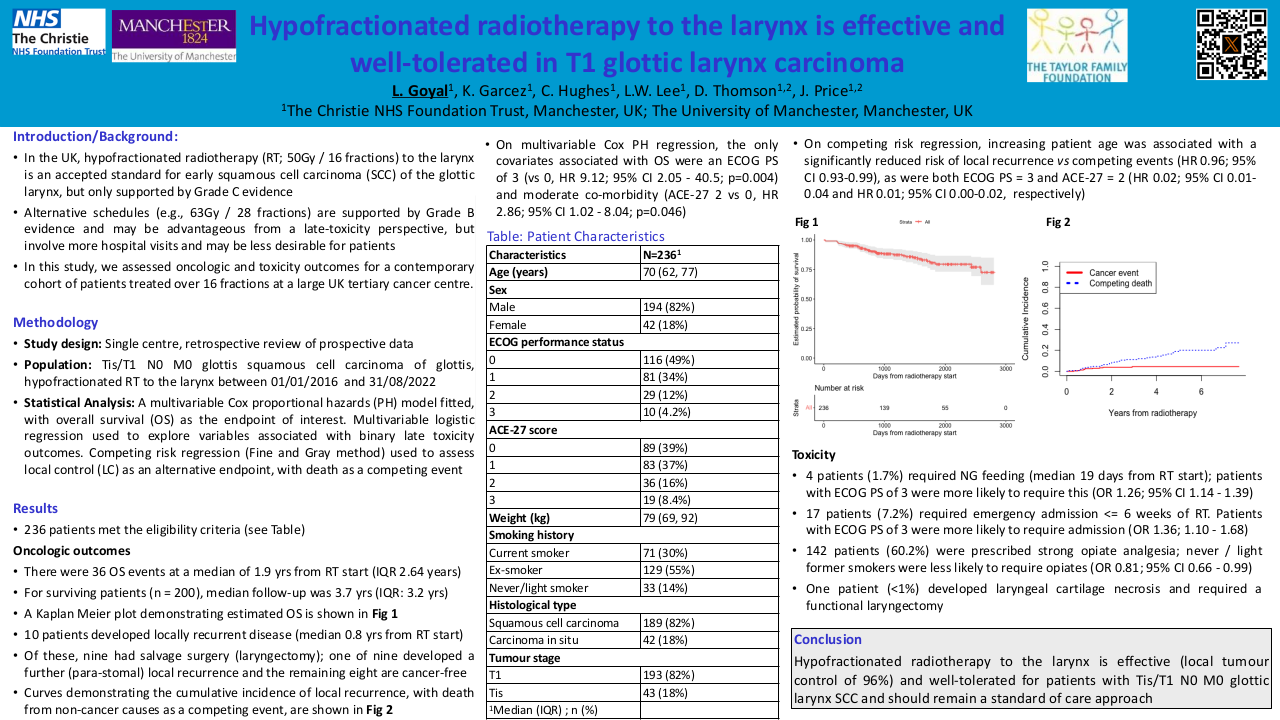
6110 patients were included in the study. Among them, 855 patients underwent 'Surgery,' 1420 patients received 'CTX' (chemotherapy), 32 had 'Surgery + CTX,' 635 patients underwent 'Surgery + ART' (adjuvant radiation therapy), 224 had 'Surgery + ART + CTX,' and 2944 received 'None.' Most patients (61.2%) were 60 years or older, with a median age of 63 years. The largest racial group was white (84.3%; n=5150). A total of 76.7% of the patients had a tumor size of 1-2 cm, followed by 17.4% for tumors > 2 cm, and 6.0% for tumors measuring < 1 cm. The median tumor size was 1.8 cm. 'Surgery' had the most favorable survival outcome with a 5-year OS of 66.1%, followed by 'Surgery + ART + CTX' (62%), 'Surgery + ART' (58%), 'None' with (48.4%), 'CTX' (47.9%), and then 'Surgery + CTX' with (36.4%). In terms of CSS, 'Surgery + ART' had the most favorable survival outcome with a 5-year CSS of 92.8%, followed by 'Surgery + CTX' (90.6%), 'Surgery + ART + CTX' (89%), 'CTX' (88%), 'Surgery' (87.1%), and then 'None' with (85.9%). Significant differences were found in OS and CSS between the therapeutic groups (P<0.0001) for both OS and CSS. Older age, male sex, 1-2 cm tumor size, > 2 cm tumor size, and 'Surgery + CTX' were poor prognostic factors for OS. Older age and tumor size of > 2 cm were poor prognostic factors for CSS. However, 1-2 a tumor size was a good prognostic factor for CSS. Multivariable analysis confirmed a statistically significant difference between the effects of all therapeutic groups on OS and CSS. Table1
| Treatment Group |
OS Hazard Ratio |
OS 95% CI |
CSS Hazard Ratio |
CSS 95% CI |
| Surgery |
0.64 | 0.57 - 0.72 |
0.82 | 0.57 - 0.89 |
| Surgery + ART |
0.68 | 0.61 - 0.77 |
0.75 | 0.67 - 0.83 |
| Surgery + ART + CTX |
0.81 | 0.68 - 0.96 |
0.80 | 0.68 - 0.94 |
Conclusion
Our study showed significant variations in the survival outcomes among patients with supraglottic SCC. Therefore, this underscores the need for personalized treatment strategies for patients with supraglottic SCC and encourages further research to validate and expand upon these results for improved outcomes in this rare cancer.