Hypofractionated radiotherapy to the larynx is effective and well tolerated in T1 glottic larynx carcinoma
Purpose/Objective
In the UK, hypofractionated radiotherapy (50 Gy in 16 fractions) to the larynx is an accepted standard for early cancer of the glottic larynx, but is only supported by Grade C evidence1-2. Alternative schedules (e.g., 63 Gy in 28 fractions) are supported by Grade B evidence, and may be advantageous from a late-toxicity perspective on account of a lower dose-per-fraction, but involve more visits to the department and may be less desirable from a patient experience perspective3.
In this study, we assessed oncologic and toxicity outcomes for a contemporary cohort of patients treated over 16 fractions at a large UK tertiary cancer centre.
Material/Methods
A retrospective review of prospectively-collected data. Eligibility criteria: all patients who completed hypofractionated radiotherapy to the larynx for Tis /T1 N0 M0 squamous cell carcinoma of the glottis at The Christie NHS Foundation Trust between 01/01/2016 and 31/08/2022. Relevant patient-, cancer- and treatment factors were collected.
A multivariable Cox proportional hazards (PH) model was fitted, with overall survival (OS) as the endpoint of interest. Multivariable logistic regression was used to explore variables associated with binary late toxicity outcomes. Competing risk regression, using the method of Fine and Gray, was used to assess local control (LC) as an alternative endpoint, with death as a competing event.
Results
236 patients met the eligibility criteria; patient characteristics are shown in the Table.
| Characteristics | N=2361 |
| Age (years) | 70 (62, 77) |
| Sex | |
| Male | 194 (82%) |
| Female | 42 (18%) |
| ECOG performance status |
|
| 0 | 116 (49%) |
| 1 | 81 (34%) |
| 2 | 29 (12%) |
| 3 | 10 (4.2%) |
| ACE-27 score |
|
| 0 | 89 (39%) |
| 1 | 83 (37%) |
| 2 | 36 (16%) |
| 3 | 19 (8.4%) |
| Unknown | 9 |
| Weight (kg) |
79 (69, 92) |
| Unknown | 85 |
| Smoking history |
|
| Current smoker |
71 (30%) |
| Ex-smoker |
129 (55%) |
| Never / light former |
33 (14%) |
| Unknown |
3 |
| Histological type |
|
| SCC |
189 (80%) |
| CIS |
42 (18%) |
| Spindle |
4 (1.7%) |
| Unknown |
1 |
| Tumour stage |
|
| T1 |
193 (82%) |
| Tis |
43 (18%) |
| Prescribed radiotherapy dose (Gy) |
|
| 50 |
196 (83%) |
| 52.5 |
40 (17%) |
| 1Median (IQR); n(%) |
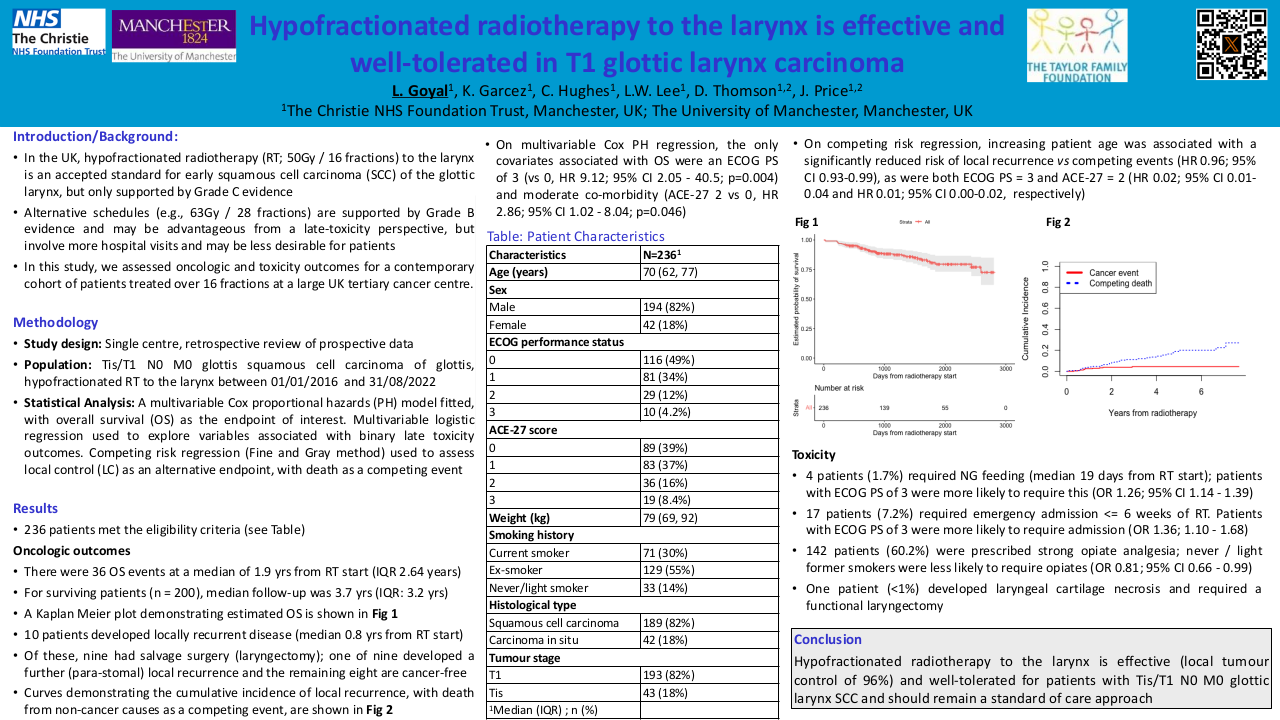
There were 36 OS events at a median of 1.9 years from radiotherapy start (IQR 2.6 years). For surviving patients (n = 200), the median follow-up was 3.7 years (IQR 3.2 years).
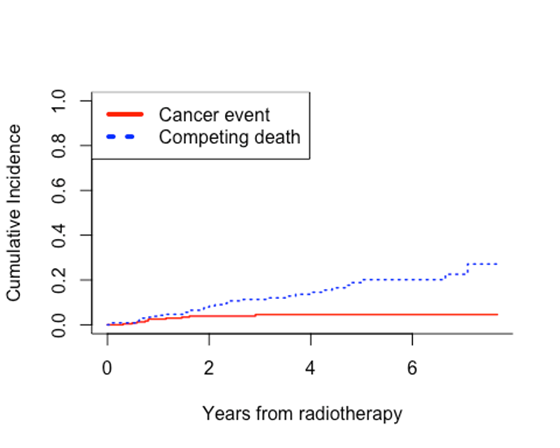
10 patients developed locally recurrent disease at a median of 0.8 years from radiotherapy start. Of these, 9 had salvage surgery (laryngectomy); 1 of 9 developed a further (para-stomal) local recurrence and 8 remain cancer-free. Curves demonstrating the cumulative incidence of local recurrence, with death from non-cancer causes as a competing event, are shown in the Figure.
On multivariable Cox PH regression, the only covariates associated with OS were an ECOG PS of 3 (vs 0, HR 9.12; 95% CI 2.05 - 40.5; p=0.004) and moderate co-morbidity (ACE-27 2 vs 0, HR 2.86; 95% CI 1.02 - 8.04; p=0.046). On competing risk regression, increasing patient age was associated with a significantly reduced risk of local recurrence vs competing events (HR 0.96; 95% CI 0.93-0.99, p<0.01), as were both ECOG PS = 3 and ACE-27 = 2 (HR 0.02; 95% CI 0.01-0.04, p<0.01 and HR 0.01; 95% CI 0.00-0.02, p<0.01 respectively).
4 patients (1.7%) required NG feeding, at a median time of 19 days from radiotherapy start (IQR 5.75 days). On logistic regression, patients with an ECOG PS of 3 were more likely to require NG insertion (OR 1.26; 95% CI 1.14 - 1.39; p<0.001). 17 patients (7.2%) required emergency inpatient admission during or within six weeks of finishing radiotherapy. Patients with an ECOG PS of 3 were more likely to require admission (OR 1.36; 95% CI 1.10 - 1.68; p=0.004). 142 patients (60.2%) were prescribed strong opiate analgesia (i.e., oral morphine solution). Never / light former smokers were less likely to be prescribed opiates (OR 0.81; 95% CI 0.66 - 0.99; p=0.042). One patient (<1%) developed laryngeal cartilage necrosis and required a functional laryngectomy.
Conclusion
Hypofractionated radiotherapy to the larynx is effective (local tumour control of 96%) and well-tolerated for patients with Tis / T1 N0 M0 squamous cell carcinoma of the glottic larynx, and should remain a standard of care approach.
1. RCR. Radiotherapy Dose fractionation, Third Edition | the Royal College of Radiologists [Internet]. www.rcr.ac.uk. 2019. Available from: https://www.rcr.ac.uk/publication/radiotherapy-dose-fractionation-third…. Le QT, Fu KK, Kroll S, Ryu JK, Quivey JM, Meyler TS, et al. Influence of fraction size, total dose, and overall time on local control of T1–T2 glottic carcinoma. 1997 Aug 1;39(1):115–26.3. Short S, Krawitz H, Macann A, West T, Morton R, McIvor N, et al. T1N0/T2N0 glottic carcinoma: A comparison of two fractionation schedules. Australasian Radiology. 2006 Apr;50(2):152–7.