14-day Pathway from Decision to Treat to Radiotherapy for Head and Neck Cancer in the National Health Service: An Evaluation of Feasibility and Outcomes at Torbay Hospital.
Purpose/Objective
In squamous cell carcinoma of the head and neck there is significant evidence that a prolonged time to treatment initiation results in worse overall survival and loco-regional control1-6. This is also evidenced in the adjuvant setting: Patients receiving radiotherapy within 11 weeks of surgery had significant improvement in loco-regional control, compared to those who waited more than 13 weeks7-11. This is reflected in NHS England and JCCO guidance12.
The primary objective of this audit was to evaluate compliance to a 14-day pathway from decision to treat (DTT) to radical radiotherapy, over a 5-year period at Torbay Hospital, UK 13. We also evaluated compliance for patients receiving postoperative radiotherapy: aiming for all patients to start adjuvant treatment within 35 days of surgery. Our secondary objective was to review survival and recurrence rates within these patients.
Material/Methods
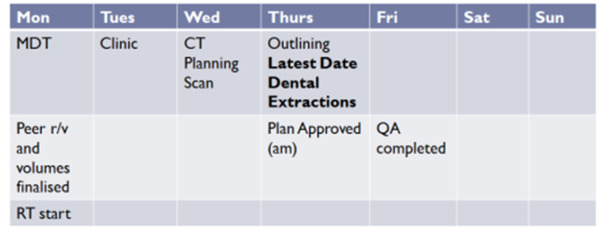
A 14-day pathway from DTT to start of radiotherapy was developed following a quality improvement project which identified common causes of delay. Key preparatory steps are scheduled to enable timely radiotherapy delivery. The pathway is demonstrated in Figure 1.
From January 2017 to December 2022, data on DTT date, site of disease, radiotherapy start date, date of surgery, date of recurrence and date of death was prospectively collected for all patients undergoing definitive radiotherapy or post-operative radiotherapy with curative intent for squamous cell carcinoma of the head and neck. Patients undergoing radiotherapy with palliative intent, patients with non-squamous cell cancers, benign pathologies and patients receiving neoadjuvant chemotherapy or targeted systemic treatment were excluded. 187 patients were included in total over the period.
Results
117 (62.6%) patients underwent radical radiotherapy within 14 days of DTT, 55 (29.4%) patients started within 15 to 21 days and 15 (8.0%) patients started after more than 22 days. Of the 75 patients receiving radiotherapy adjuvantly, 39 (52%) received radiotherapy within 35 days of surgery and 49 (65%) patients received radiotherapy within the national target of 42 days.
158 (84.5%) patients of the 187 treated within the 5-year period were alive at the end of the study period. 9 (4.8%) patients had had a local recurrence of their disease only, 17 (9.1%) patients had metastatic disease. Recurrence by site was; Larynx: 3 of 25 (12%), P16 positive oropharynx: 5 of 84 (6%), P16 negative oropharynx: 4 of 10 (40%), Oral Cavity: 7 of 26 (26.9%), Nasopharynx: 2 of 4 (50%), Parotid: 4 of 15 (26.7%), CUP: 1 of 12 (8.3%). 10 (38.4%) of the 26 patients who developed loco-regional recurrence or metastatic disease had a treatment time of more than 14 days. There was one treatment-related death due to neutropenic sepsis.
Conclusion
This audit demonstrates that a 14-day pathway for the radical treatment of squamous cell cancers of the head and neck is achievable for the majority of patients. Whilst local recurrence and survival data is not mature it is thus far in-keeping with published outcomes. Adherence to the pathway has been maintained over a prolonged period despite workload pressures within the NHS, at no extra financial cost and throughout the Covid-19 pandemic. We therefore believe this would be transferrable to other treatment centres.
1. Fortin A, Bairati I, Albert M, Moore L et al. Effect of treatment delay on outcome of patients with early-stage head-and-neck carcinoma receiving radical radiotherapy. Int J Radiat Oncol Biol Phys. 2002 Mar 15;52(4):929-36.2. van Harten MC, Hoebers FJ, Kross KW et al. Determinants of treatment waiting times for head and neck cancer in the Netherlands and their relation to survival. Oral Oncol 2015 Mar;51(3):272-8.3. Chen Z, King W, Pearcey R, Kerba M et al. The relationship between waiting time for radiotherapy and clinical outcomes: a systematic review of the literature. Radiother Oncol. 2008 Apr;87(1):3-16. 4. Polesel J, Furlan C, Birri S, Giacomarra V et al. The impact of time to treatment initiation on survival from head and neck cancer in north-eastern Italy. Oral Oncol. 2017 Apr;67:175-182. 5. Grønhøj C, Jensen D, Dehlendorff C, Nørregaard C et al. Impact of Time to Treatment Initiation in Patients with Human Papillomavirus-positive and -negative Oropharyngeal Squamous Cell Carcinoma. Clin Oncol (R Coll Radiol). 2018 Jun;30(6):375-381.6. Dalke et al. Impact of Time Factors on Outcome in Patients with Head and Neck Cancer Treated with Definitive Radio(Chemo)Therapy. Sep-Oct;31(5):949-955. In Vivo. 2017.7. Byers RM, Clayman GL, Guillamondequi OM et al. Resection of advanced cervical metastasis prior to definitive radiotherapy for primary squamous carcinomas of the upper aerodigestive tract. Head Neck. 1992 Mar-Apr;14(2):133-8.8. Peters LJ, Goepfert H, Ang KK, Byers RM et al. Evaluation of the dose for postoperative radiation therapy of head and neck cancer: first report of a prospective randomized trial. Int J Radiat Oncol Biol Phys. 1993 Apr 30;26(1):3-11.9. Ang KK, Trotti A, Brown BW, Garden AS et al. Randomized trial addressing risk features and time factors of surgery plus radiotherapy in advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2001 Nov 1;51(3):571-8.10. Tribius S, Donner J, Pazdyka H, Münscher A et al. Survival and overall treatment time after postoperative radio(chemo)therapy in patients with head and neck cancer. Head Neck. 2016 Jul;38(7):1058-65. 11. Graboyes EM, Garrett-Mayer E, Ellis MA, Sharma AK et al. Effect of time to initiation of postoperative radiation therapy on survival in surgically managed head and neck cancer. Cancer. 2017 Dec 15;123(24):4841-4850.12. House of Commons Committee of Public Accounts ‘NHS waiting times for elective and cancer treatment’ One Hundredth Report of Session 2017–19. HC 1750 Published on 12 June 2019.13. Cope V, Chambers J, Kingdon S, Cole N. Is a 14-day Pathway From Decision to Treat to Radiotherapy for Head and Neck Cancer Patients Feasible in the National Health Service? The Torbay Experience 5 Years On. Clinical Oncology. 2023:35 (11) 756-758.