Acute swallowing outcomes in oropharyngeal cancers following clinical introduction of dysphagia-optimised IMRT (DO-IMRT) at a single tertiary centre
Purpose/Objective
Swallowing dysfunction following curative (chemo) radiotherapy (RT) for head and neck cancers (HNC) is a significant treatment-related morbidity. Dysphagia-optimised IMRT (DO-IMRT) has recently shown to improve patient-reported swallowing outcomes, by reducing RT dose to dysphagia and aspiration – related structures. We implemented DO-IMRT in HNC patients undergoing primary radical RT-based treatment at our institution in August 2021. The objective of this retrospective analysis was to evaluate patient-reported and physician-scored acute swallowing toxicities in oropharyngeal squamous cell carcinoma (OPSCC) treated with DO-IMRT.
Material/Methods
Eligibility criteria included newly diagnosed OPSCC, treatment with primary radical DO-IMRT to the oropharynx and bilateral neck, alive and with no evidence of loco-regional recurrence at a minimum of 6 months following treatment completion. All patients received 65 Gy/30 fractions/6 weeks to the planning target volume (PTV1) of the tumour and involved nodes and 54 Gy/30 fractions/6 weeks to regions at risk of microscopic disease (PTV2) +/- chemotherapy as per institutional guidelines. Volumes of extended oral cavity, superior pharyngeal constrictor (PC), middle PC, inferior PC and larynx lying outside the PTVs were set optimal mean dose constraints of < 40 Gy, < 50 Gy, < 50 Gy, < 50 Gy, and < 30 Gy respectively during the optimisation process. Under-dosage of PTVs was not permitted to meet optimal dose constraints. Patients prospectively completed MD Anderson dysphagia inventory (MDADI), a patient-reported swallowing questionnaire, at baseline, week 6 , 3 –, 6 –, 12 – and 24 months following treatment completion and a composite MDADI score for each point was generated. Prospective physician-scored toxicities using CTCAE v5.0 were also recorded at the above timepoints. This analysis evaluated swallowing outcomes measures upto 6 months post-RT. Descriptive statistics were used to report results.
Results
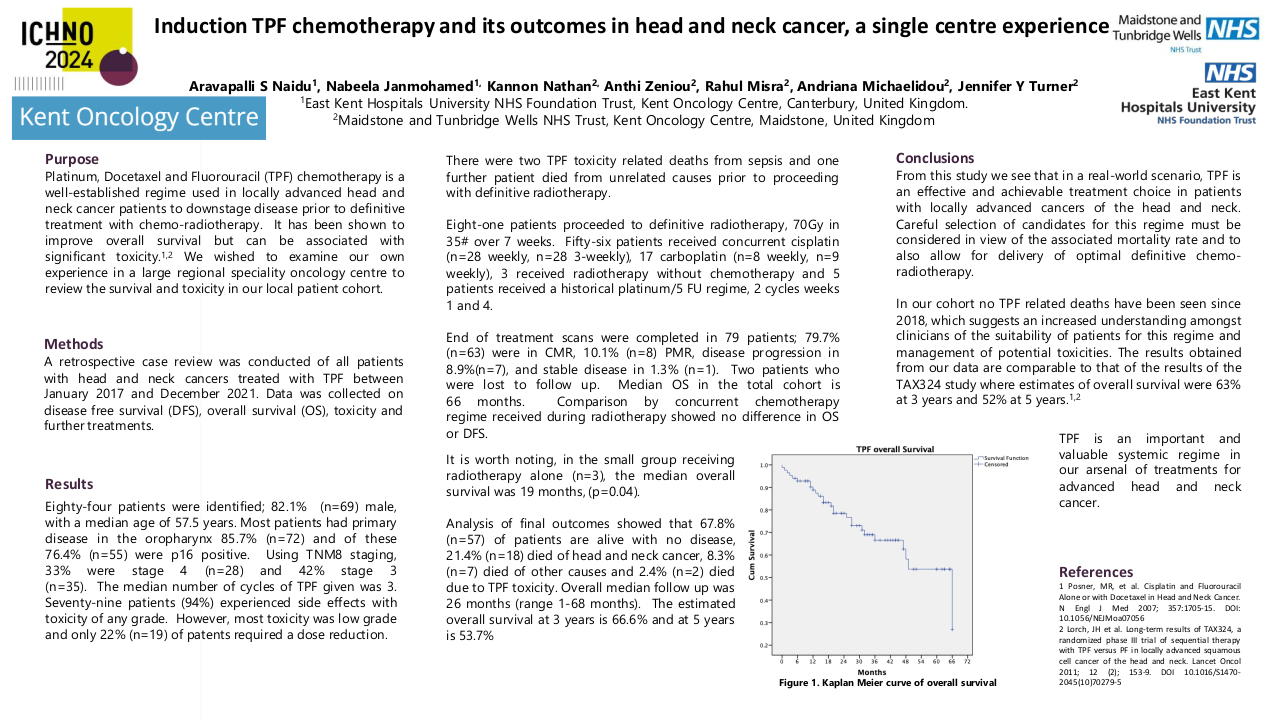
47/56 OPSCC patients treated between August 2021 and February 2023 met the eligibility criteria. Baseline patient and tumour characteristics are presented in table 1. Majority of tumours were stage IV (AJCC 7thedition), human papillomavirus-associated, and treated with concomitant CRT. Mean (SD) composite MDADI scores at baseline, week 6, 3- and 6- months post treatment were 84 (15.0), 55.4 (12.8), 66.1 (18.3) and 73.1 (19.1) respectively (Table 2). Compared to baseline, 7 % and 11 % of patients reported a 10-point (clinically significant) improvement in composite MDADI score at 3 and 6 months respectively. The proportion of patients recording a clinically significant worse score was 87 %, 67 % and 53 % at week 6, and at 3- and 6 – months. 18 (38 %) patients required feeding tube (FT) insertion. 2 (4 %) patients were FT- dependent at 6 months. Majority of patients (81 %) had < grade 2 dysphagia at 6 months.
Table 1 : Baseline characteristics
|
Characteristics |
|
|
Sex |
|
|
Male |
32 (68 %) |
|
Female |
15 (32 %) |
|
|
|
|
Age at diagnosis |
|
|
Median |
62 |
|
Range |
51 - 77 |
|
|
|
|
Tumour subsite |
|
|
Base of tongue |
15 (32 %) |
|
Tonsil |
27 (57 %) |
|
Soft palate |
5 (11 %) |
|
|
|
|
HPV status |
|
|
Positive |
38 (81 %) |
|
Negative |
9 (19%) |
|
|
|
|
Smoking history |
|
|
Never |
13 (28 %) |
|
< 10 pack year |
11 (23 %) |
|
> 10 pack year |
21 (45 %) |
|
Unknown |
2 (4 %) |
|
|
|
|
Tumour staging |
|
|
T1 |
5 (11 %) |
|
T2 |
9 (19%) |
|
T3 |
7 (15 %) |
|
T4 |
26 (55 %) |
|
|
|
|
Nodal staging (AJCC 7th edition) |
|
|
N0 |
10 (20 %) |
|
N1 |
6 (13 %) |
|
N2a |
6 (13 %) |
|
N2b |
13 (28 %) |
|
N2c |
7 (15 %) |
|
N3 |
5 (11 %) |
|
|
|
|
TNM staging |
|
|
I |
1 (2 %) |
|
II |
4 (9 %) |
|
III |
3 ( 6%) |
|
IV |
39 (83 %) |
|
|
|
|
Treatment |
|
|
CRT |
34 (72%) |
|
IC + CRT |
4 (9 %) |
|
RT |
9 (19 %) |
|
Composite MDADI score |
N with data |
Mean |
SD |
|
Baseline |
47 |
84 |
15.0 |
|
Week 6 |
45 |
55.4 |
12.8 |
|
3 months post - RT |
42 |
66.1 |
18.3 |
|
6 months post – RT |
46 |
73.1 |
19.1 |
|
|
|
|
|
|
Change – Baseline to week 6 |
45 |
-28.5 |
16.8 |
|
Change – Baseline to 3 months |
42 |
-18.3 |
17.1 |
|
Change – Baseline to 6 months |
46 |
-11.1 |
18.4 |
Table 2 : MDADI composite scores at different timepoints
Conclusion
FT-dependence in this initial cohort of OPSCC patients treated with DO-IMRT at our centre is low and compares favourably to contemporary data. Swallowing-related quality of life outcomes appear promising, with incremental improvements at 3- and 6-months post treatment. Future work includes assessment of longitudinal toxicity data, and the relationship between RT dose swallowing structures and toxicity.
1. Nutting C, Finneran L, Roe J, Petkar I, Rooney K, Hall E, et al. Dysphagia-optimised intensity-modulated radiotherapy versus standard radiotherapy in patients with pharyngeal cancer. Lancet Oncol. 2023;24(10):e398.