Can machine-learning model predict overall survival in head and neck cancer patients?.
Purpose/Objective
To be able through a machine learning model, to predict overall survival in patients with head and neck cancer treated with curative intent in our centre between July 2018 and December 2022. Patients were treated with radiotherapy +/- chemotherapy with curative intent or surgery plus adjuvant radiotherapy.
Material/Methods
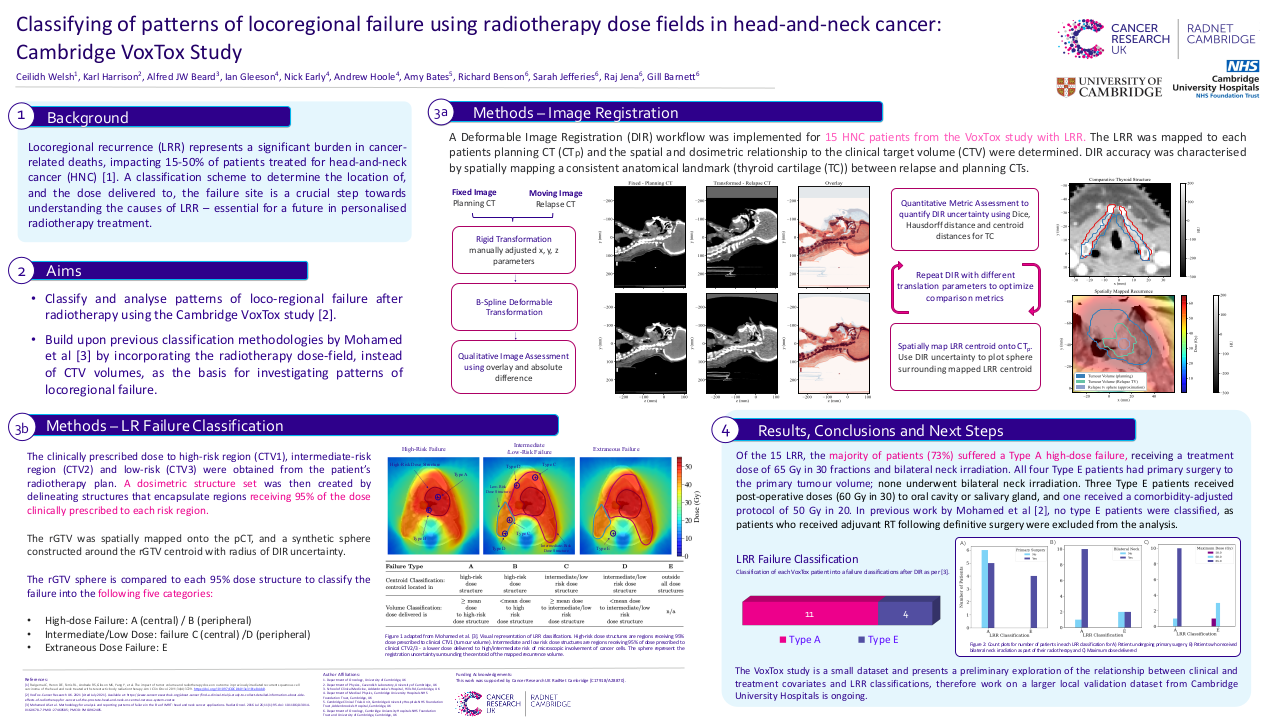
A machine learning model (Classification and Regression Trees (CRT)) and a deep learning model (Multilayer Perceptron (MLP)) were used to predict overall survival based on some clinical characteristics as well as dosimetric characteristics of our radiotherapy treatment.
404 patients with head and neck cancer (HANC) of different sublocations (extracted from a real-world database build with variables generated through the MOSAIQ (Elekta) corporate system of the Andalusian Health System) were used. Status alive or dead in October 2023 was known in all of them.
Those who received a dose equal to or greater than 50 Gy to CTV_BED or CTV_T were finally selected to transformation (n= 342 patients).
They were randomly into a training cohort (n=236) and a test cohort (n=106) according to a 7:3 ratio. The variables were selected after an exploratory Factor Analysis: Principal Component Analysis (PCA) and were analyzed and transformed (standardization and obtaining z values) to improve sample quality.
The receiver operating characteristic curve (ROC), Kaplan Meier curve and C-index were used to display the capability to prediction of the constructed models.
Results
Twenty clinical and dosimetric characteristics were evaluated and transformed for exploratory PCA analysis. Those with multicollinearity problems were excluded. Finally, they were selected: status, tumor sublocation, morphology, total prescribed dose, mean dose at PTV, PTV volume, fractions, total treatment time and theoretical total treatment time.
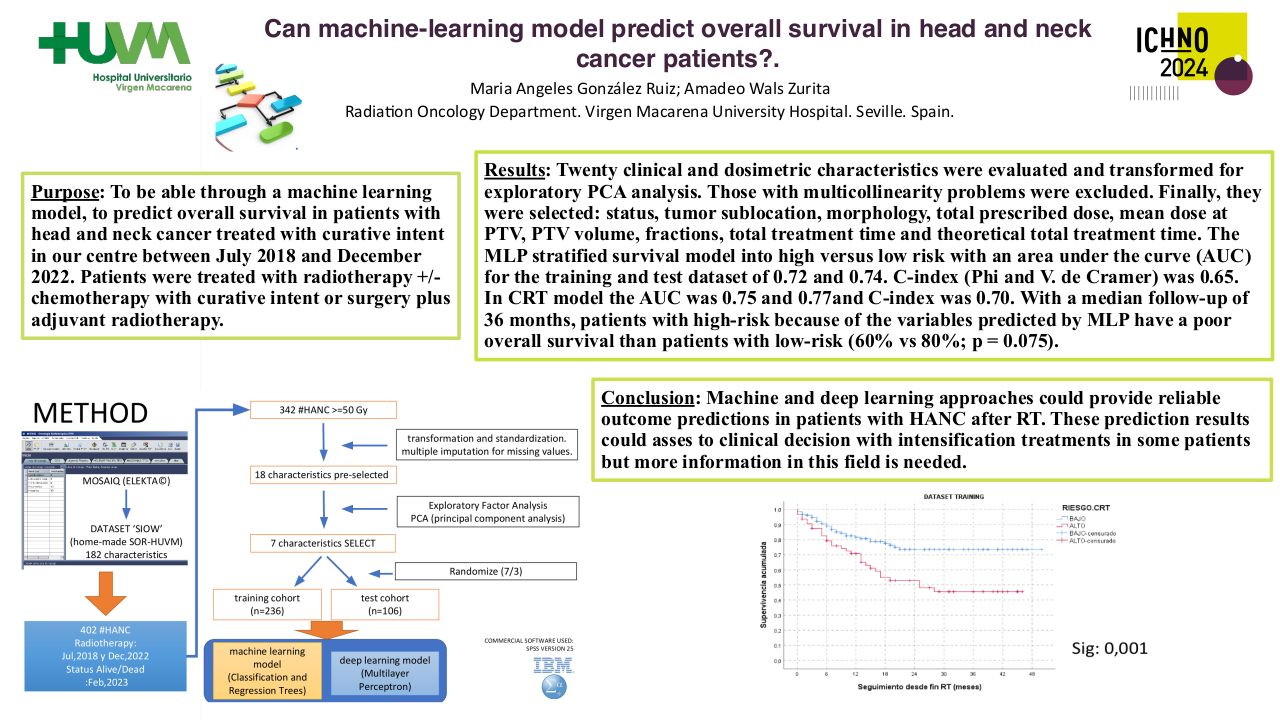
The MLP stratified survival model into high versus low risk with an area under the curve (AUC) for the training and test dataset of 0.72 and 0.74. C-index (Phi and V. de Cramer) was 0.65.
In CRT model the AUC was 0.75 and 0.77and C-index was 0.70.
With a median follow-up of 36 months, patients with high-risk because of the variables predicted by MLP have a poor overall survival than patients with low-risk (60% vs 80%; p = 0.075).
Conclusion
Machine and deep learning approaches could provide reliable outcome predictions in patients with HANC after RT. These prediction results could asses to clinical decision with intensification treatments in some patients but more information in this field is needed.