Implementation challenges of artificial intelligence-based radiomics in head and neck oncology: A systematic review
Purpose/Objective
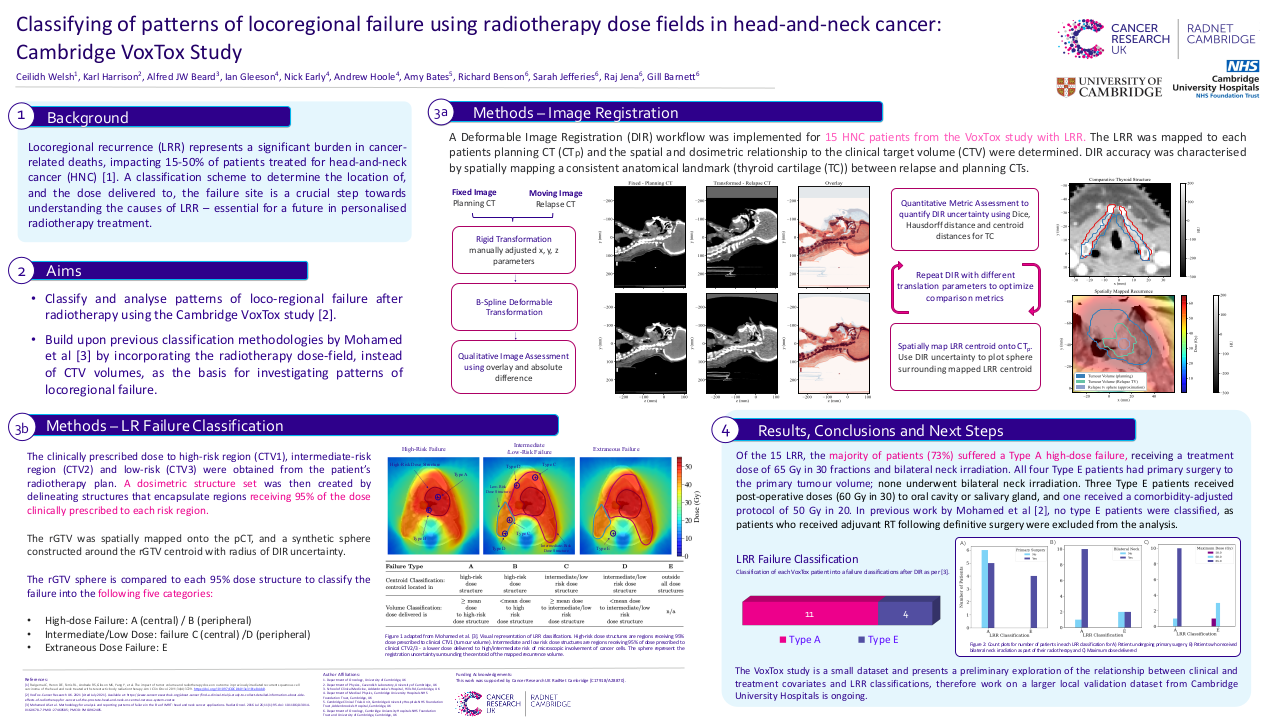
Purpose/Objectives: Artificial intelligence (AI) and its subfields such as machine learning (ML) and deep learning (DL) have been reported to show high performance, particularly in the diagnosis and prognosis of various cancers 1–3. Despite the promising results obtained from these studies, advancements in technology have increased the availability of medical images in different formats such as computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), and ultrasound images 1,2. Interestingly, these image formats are more than pictures, they are in fact, data 4. As a result, several approaches such as radiomics have been recently used to extract information that is not visible to the human eye during routine examination from these images 5. Hence, radiomics is an emerging field in radiology that provides a non-invasive approach for extracting quantitative features from medical cancer images such as CT, PET, MRI, or a combination of these image formats 5. Traditionally, the extracted features are processed using statistical approaches. However, due to the large amount of extracted features, statistical approaches can no longer effectively handle these features 6,7. Therefore, in recent years, several studies exploring the potential of AI or its subfields such as ML and DL in handling the extracted features to produce a predictive model have shown promising results that are capable of revolutionizing HNC management 8. However, in actual everyday clinical practice, the use of AI-based radiomics models remains limited 5. This is due to several implementation challenges 5. Objectives: This study provides a systematic review of the challenges, concerns, and limitations of AI-based models in head and neck cancer (HNC) oncology. Furthermore, we suggest possible solutions to these challenges.
Material/Methods
We searched OvidMedline, PubMed, Scopus, and Web of Science databases for articles that examine the challenges of AI-based models in HNC oncology. The quality of included studies and their risk of biases were evaluated using the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) and Prediction Model Risk of Bias Assessment Tool (PROBAST).
Results
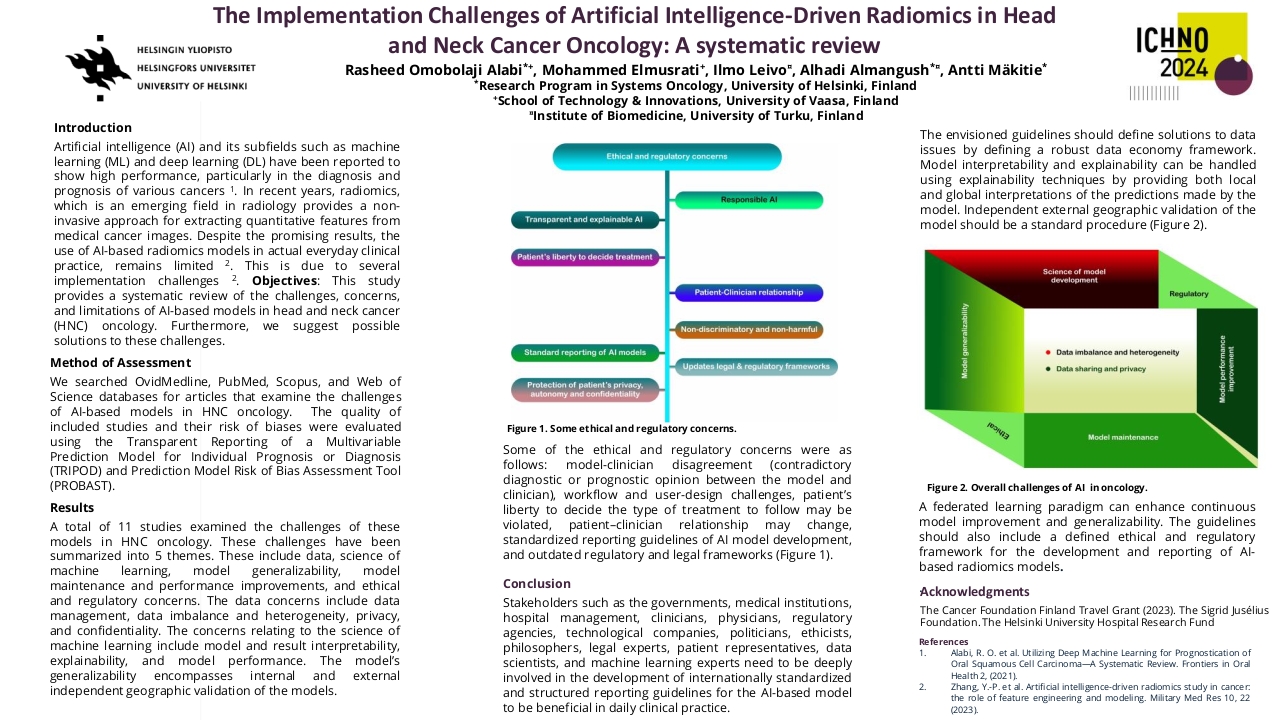
A total of 11 studies examined the challenges of these models in HNC oncology. These challenges have been summarized into 5 themes. These include data, science of machine learning, model generalizability, model maintenance and performance improvements, and ethical and regulatory concerns. The data concerns include data management, data imbalance and heterogeneity, privacy, and confidentiality. The concerns relating to the science of machine learning include model and result interpretability, explainability, and model performance. The model’s generalizability encompasses internal and external independent geographic validation of the models. Some of the ethical and regulatory concerns were as follows: model-clinician disagreement (contradictory diagnostic or prognostic opinion between the model and clinician), workflow and user-design challenges, patient’s liberty to decide the type of treatment to follow may be violated, patient–clinician relationship may change, standardized reporting guidelines of AI model development, and outdated regulatory and legal frameworks.
Conclusion
Stakeholders such as the governments, medical institutions, hospital management, clinicians, physicians, regulatory agencies, technological companies, politicians, ethicists, philosophers, legal experts, patient representatives, data scientists, and machine learning experts need to be deeply involved in the development of internationally standardized and structured reporting guidelines for the AI-based model to be beneficial in daily clinical practice. The envisioned guidelines should define solutions to data issues by defining a robust data economy framework. Model interpretability and explainability can be handled using explainability techniques by providing both local and global interpretations of the predictions made by the model. Independent external geographic validation of the model should be a standard procedure. A federated learning paradigm can enhance continuous model improvement and generalizability. The guidelines should also include a defined ethical and regulatory framework for the development and reporting of AI-based radiomics models.
1. Alabi, R. O. et al. Utilizing Deep Machine Learning for Prognostication of Oral Squamous Cell Carcinoma—A Systematic Review. Frontiers in Oral Health 2, (2021).2. Alabi, R. O., Almangush, A., Elmusrati, M. & Mäkitie, A. A. Deep Machine Learning for Oral Cancer: From Precise Diagnosis to Precision Medicine. Front. Oral. Health 2, 794248 (2022).3. Alabi, R. O. et al. Application of artificial intelligence for overall survival risk stratification in oropharyngeal carcinoma: A validation of ProgTOOL. International Journal of Medical Informatics 175, 105064 (2023).4. Gillies, R. J., Kinahan, P. E. & Hricak, H. Radiomics: Images Are More than Pictures, They Are Data. Radiology 278, 563–577 (2016).5. Zhang, Y.-P. et al. Artificial intelligence-driven radiomics study in cancer: the role of feature engineering and modeling. Military Med Res 10, 22 (2023).6. Kocak, B. et al. Radiomics with artificial intelligence: a practical guide for beginners. Diagn Interv Radiol 25, 485–495 (2019).7. Alabi, R. O. et al. Machine learning in oral squamous cell carcinoma: Current status, clinical concerns and prospects for future—A systematic review. Artificial Intelligence in Medicine 115, 102060 (2021).8. Haider, S. P., Burtness, B., Yarbrough, W. G. & Payabvash, S. Applications of radiomics in precision diagnosis, prognostication and treatment planning of head and neck squamous cell carcinomas. Cancers Head Neck 5, 6 (2020).