Classifying of patterns of locoregional failure using radiotherapy dose fields in head-and-neck cancer: Cambridge VoxTox Study
Purpose/Objective
Locoregional recurrence (LRR) represents a significant burden in cancer-related deaths, impacting 15-50% of patients treated for head-and-neck cancer (HNC) [1]. Accurately classifying the location of, and the dose delivered to, the failure site is a crucial step towards understanding the causes of LRR. The aim of this study is to classify and analyse patterns of loco-regional failure after radiotherapy treatment, for HNC patients, in the Cambridge VoxTox study. This classification methodology builds upon previous work done by Mohamed et al [2] by incorporating the radiotherapy dose-field, instead of CTV volumes, as the primary basis for investigating patterns of locoregional failure.
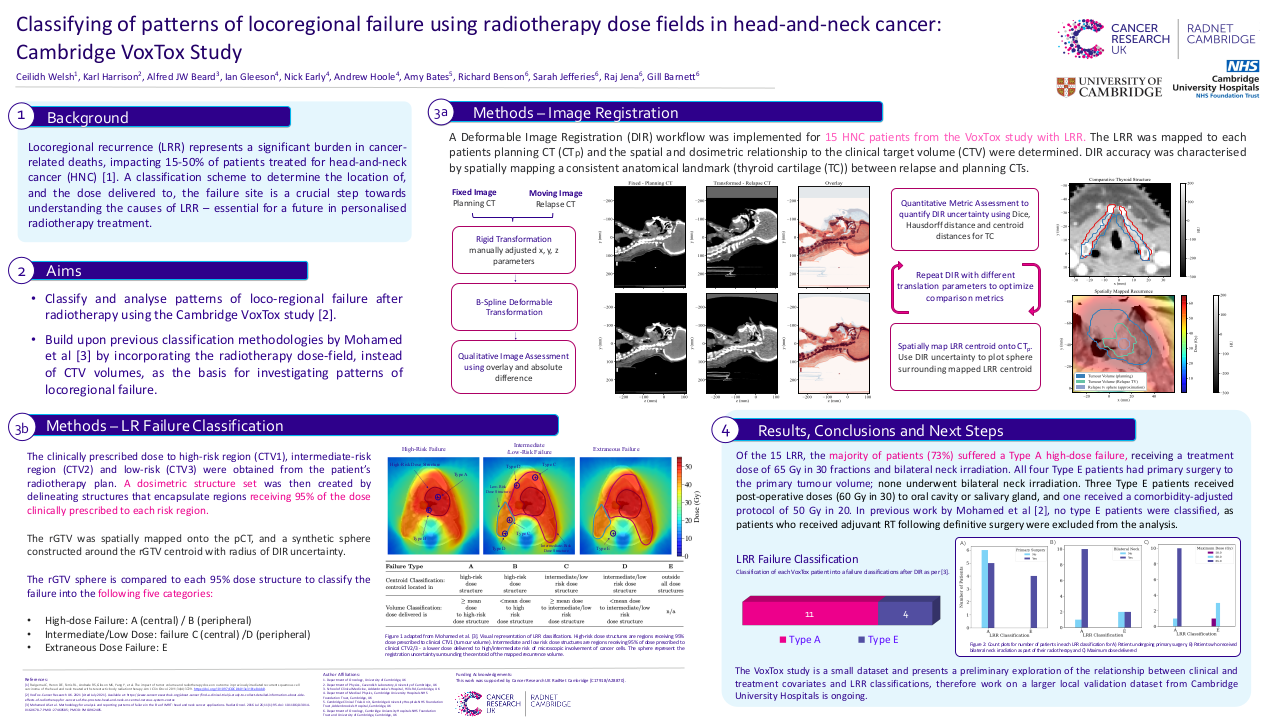
Material/Methods
Eighteen patients with evidence of local and/or locoregional failure following image-guided intensity-modulated radiotherapy (IMRT) for HNC were identified. Three patients were excluded from the analysis due to incomplete data. The relapse gross tumour volume (rGTV) and clinical target volumes (CTVs) were manually delineated on each patient’s relapse diagnostic CT (rCT) by radiation oncologists. The thyroid cartilage (TC) was delineated by experienced HNC clinicians as a comparative organ at risk (OAR) on both the planning CT (pCT) and relapse diagnostic CT (rCT). The pCT was co-registered with the rCT using deformable image registration (DIR) to obtain the transform for spatial mapping between the two CT scans. The accuracy of the DIR for each patient was quantified using the target registration error (TRE) of the centroid of the thyroid cartilage (TC). The final cohort TRE was calculated as the absolute distance between centroid of TC on the pCT and centroid of TC mapped from the rCT to the pCT, averaged across all LRR patients included in the analysis. The clinically prescribed dose to the high-risk region (CTV1), intermediate-risk region (CTV2) and low-risk region (CTV3) was obtained from the patient’s radiotherapy plan. A dosimetric structure set was then created by delineating structures that encapsulate regions receiving 95% of the dose clinically prescribed to these high-risk, intermediate-risk and low-risk CTVs. The rGTV was then spatially mapped onto the pCT and compared with each of the 95% dose structures using centroid and volume-based criteria. The failure was then classified into one of five categories, dependent on these criteria: A (central high dose), B (peripheral high dose), C (central elective dose), D (peripheral elective dose), and E (extraneous dose) [2]. Clinical patient variables were used to search for associations between treatment type and LRR classifications.
Results
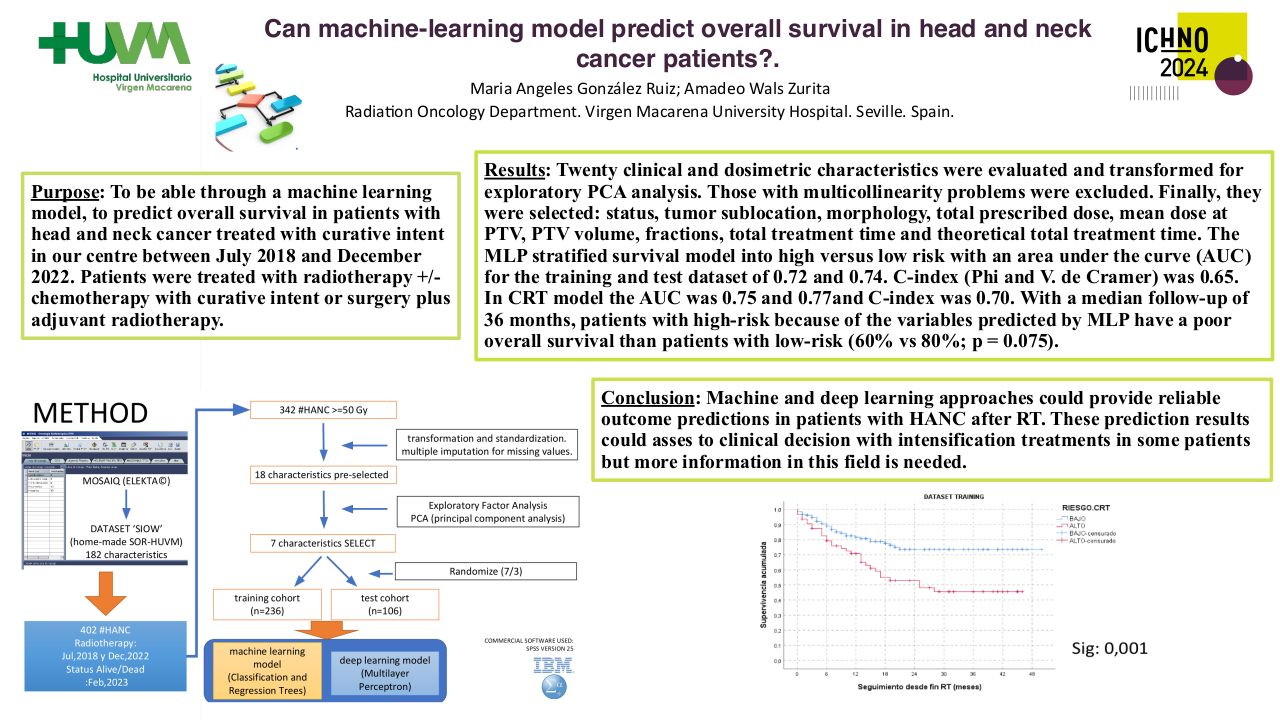
In total, 15 recurrences were identified and classified using DIR methods. The cohort DIR TRE was evaluated as 4.5 mm. Of the 15 LRR, 9 were identified as Type A (central high dose), 1 as Type B (peripheral high dose), 1 as Type C (central elective dose), and 4 as Type E (extraneous dose). Among the 9 high-risk Type A failures, 8 received 65 Gy in 30 fractions with bilateral neck irradiation, and 1 received post-operative doses of 60 Gy in 30 with unilateral neck. The most common Type A primary site was oropharynx (67%). All Type E patients had primary surgery to the primary tumour volume; none underwent bilateral neck irradiation. Three Type E patients received post-operative doses (60 Gy in 30) to oral cavity or salivary gland, and one received a comorbidity-adjusted protocol of 50 Gy in 20. Oral cavity was the primary site for 75% of Type E patients. In previous work by Mohamed et al [2], no type E patients were classified, as patients who received adjuvant RT following definitive surgery were excluded from the analysis.
Conclusion
The majority of HNC LRRs in the VoxTox study originate within the high-dose volumes (Type A), with the majority receiving a maximal treatment dose of 65 Gy in 30 fractions. Type A, high-dose, classifications are suggestive of radiobiological resistance to treatment dose. Patients recurring in the extraneous dose regions (Type E), all received primary surgery with unilateral or no neck irradiation. The VoxTox study is a small dataset and presents a preliminary exploration of LRR classifications. However, exploration in large datasets is crucial for investigating relationships between LRR failure patterns and clinical variables. As a result, work on a larger local validation dataset from Cambridge University Hospitals is ongoing.
[1] Rwigema JC, Heron DE, Ferris RL, Andrade RS, Gibson MK, Yang Y, et al. The impact of tumor volume and radiotherapy dose on outcome in previously irradiated recurrent squamous cell carcinoma of the head and neck treated with stereotactic body radiation therapy. Am J Clin Oncol. 2011;34(4):372–9. https://doi.org/10.1097/COC.0b013e3181e84dc0.[2] Mohamed AS, Rosenthal DI, Awan MJ, Garden AS, Kocak-Uzel E, Belal AM, El-Gowily AG, Phan J, Beadle BM, Gunn GB, Fuller CD. Methodology for analysis and reporting patterns of failure in the Era of IMRT: head and neck cancer applications. Radiat Oncol. 2016 Jul 26;11(1):95. doi: 10.1186/s13014-016-0678-7. PMID: 27460585; PMCID: PMC4962405.