Functional outcome after Locally Advanced Tongue cancer resections by Pull-through approach: Study from a tertiary cancer care center.
Purpose/Objective
Oral SCC (OSCC) is the eighth most prevalent cancer in the world. [1] Head and neck cancer account for more than 650,000 cases and 330,000 deaths annually worldwide. India is the world capital accounting for one-third of the global burden.[2] About 60–80% of the patients in India suffering from oral cancer are detected in the advanced stages with tongue malignancies invariably involving floor of mouth (FOM) either by primarily or forming the base of resection.[3,4]
Advanced oral cavity lesions, particularly that of tongue and FOM are associated with morbidities like speech, swallowing and breathing difficulty.[5] Hence, a balance between adequate oncological margins and optimal functional outcome is a challenge.
Mandibular lip-split and the pull-through are the two commonly used surgical techniques.[6-8] High recurrence rates of 30% with lip-split approach has led us to opt for a more secure radical approach.[9] Para-hyoid region zone is the most common site of early recurrence which is neither included in the dissection specimen nor accessible by trans-oral approach.[10] Therefore, the pull-through technique was devised for en-bloc resection of tongue cancers with cervical lymphatics. We aim to assess the oncological and functional of this Pull-through technique in locally advanced Tongue and FOM cancers.
Material/Methods
A retrospective observational study was done for patients operated in the institute from Jan 2021 - Jan 2023. 75 patients with locally advanced carcinoma tongue or FOM undergoing resection by pull through approach were included in the study.
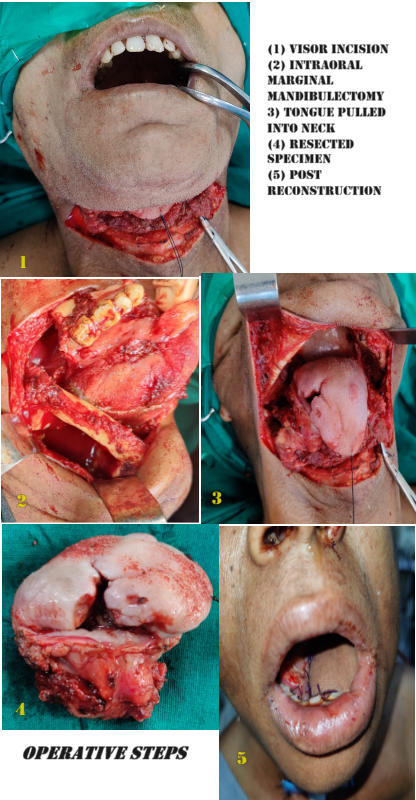
Surgical Technique (Image1: attachment)
In this technique, the Visor approach was used and Subplatysmal skin flaps raised. Bilateral level IA/IB dissection was performed, and the suprahyoid muscles divided from their bony attachment to enter the oral cavity. Subsequently, the gingivo-labial sulcus was incised on either side carefully considering for the margins and the tongue was dropped into the neck, thereby providing access to all parts of the tongue and oropharynx. Mandibulectomy, if required, was done beforehand intraorally delivering the segment with the specimen in toto. Resection and reconstruction was then performed under direct vision. Reconstruction was done either with pedicled or free flap insertion. Reattachment of the digastric muscles or remnant genioglossus, and geniohyoid muscles on both sides with the flap was done to reconstruct the floor.
Post‑operative Follow‑Up
Patients were followed up postoperatively and received adjuvant treatment as per NCCN guidelines and were provided with rehabilitatory support. Six months after the treatment, Speech, swallowing, and breathing was assessed using HNC FIT (Functional Integrity) scales.[11,12]
Results
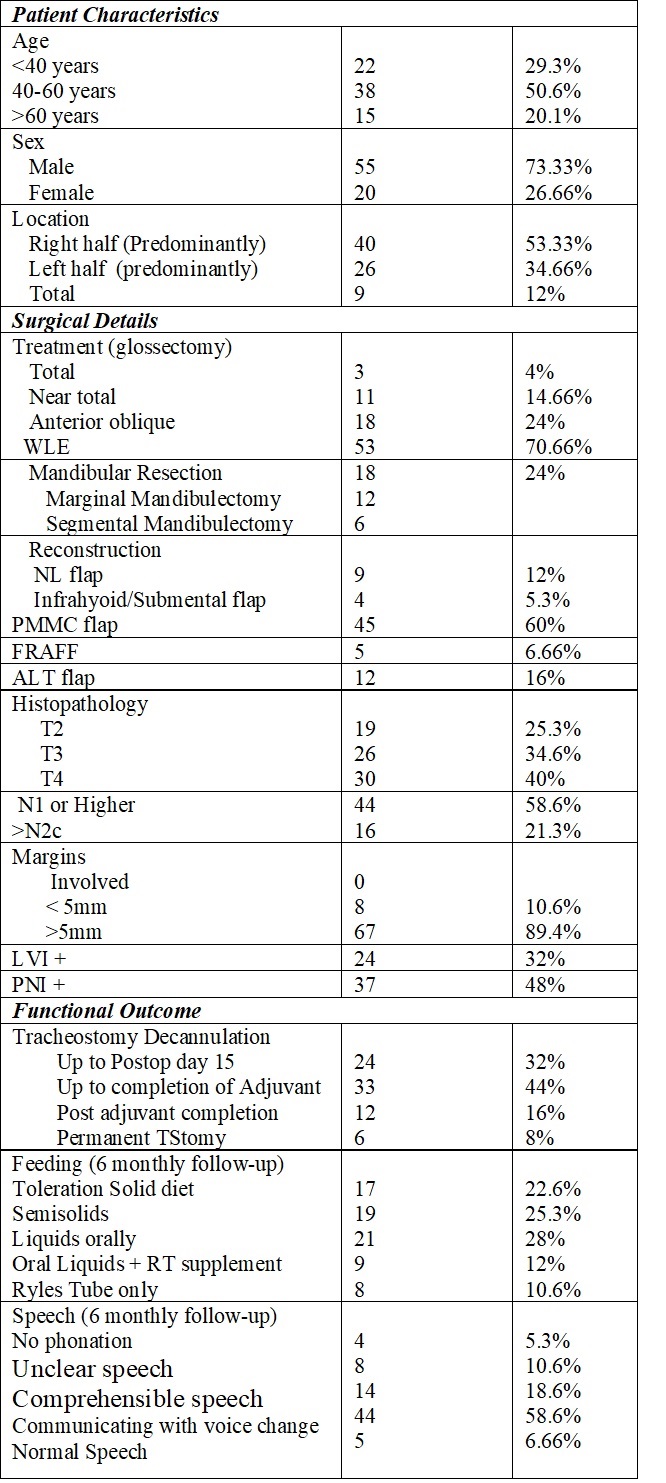
Patient Characteristics
A total of 75 patients were included in the study with 55 (73.33%) males and 20 (26.66%) females with a mean age of 47 years (range 30–76 years).
Procedural parameters
Out of a total of 75 patients, 3(4%) underwent total glossectomy, 11(14.66%) near total and 18(24%) anterior oblique glossectomy. 18 of the 75 patients underwent mandibular resections (6 - segmental and 12- marginal).
Histopathology
19 patients had T2 lesions, 26 T3 lesions and 30 T4 primaries. 31 patients (41.3%) had node negative disease while 44 (58.6%) were node positive with 16 having positive contralateral neck nodes. 24 of 75 patients (32%) had lympho-vascular invasion while 37 (48%) had perineural invasion.
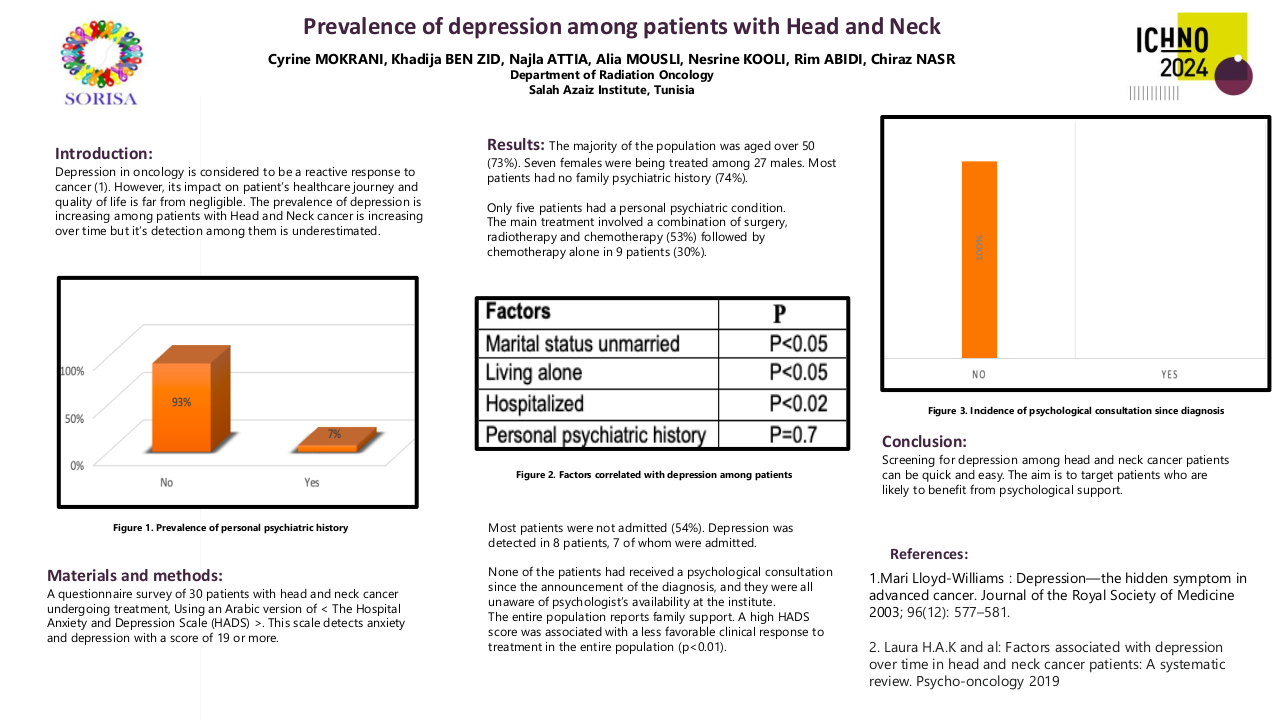
Functional outcome
As an institutional protocol, all patients undergoing major tongue resections were tracheostomised. The median duration of tracheostomy removal was 15th postop day (1st Follow-up) and 57(76%) patients were tracheostomy free by the completion of adjuvant treatment. However, 6(8%) patients had permanent tracheostomies.
Ryle’s tube feeding was started postoperatively escalating to oral feeds by POD5. Swallowing and speech rehabilitation was provided and on 6 monthly follow up, 17 of 75 (22.5%) patients tolerated solid food (HNCFIT food intake grade 3), 19 (25.3%) soft and 21 (28%) liquid diet, a total of 40 (53.3%) patients in grade 2.
9 (12%) patients required Ryle’s tube due to inadequate oral intake (grade 1), while 8 (10.6%) were entirely dependent on tube feeds (grade 0).
Out of 75 patients, 4 (5.3%) had no phonation (HNCFIT grade0), 8(10.5%) unclear speech (Grade1), 14(18.66%) had comprehensible speech with telephoning possible (grade 2), 44 (58.6%) had understandable speech with voice change(grade3), 5(6.66%) had normal voice (grade 4).
Conclusion
The pull-through approach had the advantages of good accessibility and functional outcome and ensures resection with adequate margins. Effective surgical treatment can contribute to the improved quality and length of survival of these patients.
1. Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394. 2. Laprise C., Shahul H.P., Madathil S.A., Thekkepurakkal A.S., Castonguay G., Varghese I., Shiraz S., Allison P., Schlecht N.F., Rousseau M.C., Franco E.L., Nicolau B. Periodontal diseases and risk of oral cancer in Southern India: results from the HeNCe Life study. Int. J. Canc. 2016;139:1512–1519. doi: 10.1002/ijc.30201.3. Borse V, Konwar AN, Buragohain P. Oral cancer diagnosis and perspectives in India. Sens Int. 2020;1:100046. doi: 10.1016/j.sintl.2020.100046. Epub 2020 Sep 24. PMID: 34766046; PMCID: PMC7515567. 4. Sharma S., Satyanarayana L., Asthana S., Shivalingesh K.K., Goutham B.S., Ramachandra S. Oral cancer statistics in India on the basis of first report of 29 population-based cancer registries. J. Oral Maxillofac. Pathol. 2018;22:18–26. doi: 10.4103/jomfp.JOMFP_113_175. Devine JC, Rogers SN, McNally D, Brown JS, Vaughan ED (2001) A comparison of aesthetic, functional and patient subjective outcomes following lip-split mandibulotomy and mandibular lingual releasing access procedures. Int J Oral Maxillofac Surg 30(3):199–2006. Baek, C.H.; Lee, S.W.; Jeong, H.S. New modification of the mandibulotomy approach without lip splitting.Head Neck 2006, 28, 580–586.7. Butler FS, Harrigan WF. Radical surgery for intraoral cancer with preservation of the mandible: the en bloc pull-through procedure. Am J Surg 1957: 94: 857–864.8. Cheng SJ, Ko HH, Lee JJ, Kok SH. Comparison of long-term outcomes between pull-through resection and mandibular lip-split surgery for T4a tongue/floor of mouth cancers. Head Neck 2018: 40: 144–153.9. Tsai MS, Lai CH, Lee CP, et al. Mortality in tongue cancer patients treated by curative surgery: a retrospective cohort study from CGRD. Peer J. 2016;4:e2794. 10. Başerer N. New Pull Through Resection Technique in Tongue and Floor-of Mouth Cancers. J Dent Oral Biol. 2017; 2(10): 1069.11. Dejaco D, Riedl D, Gasser S, Schartinger VH, Innerhofer V, Gottfried T, Steinbichler TB, Riechelmann F, Moschen R, Galvan O, Stigler R, Gassner R, Rumpold G, Lettenbichler-Haug A, Riechelmann H. A Tool for Rapid Assessment of Functional Outcomes in Patients with Head and Neck Cancer. Cancers (Basel). 2021 Nov 3;13(21):5529. doi: 10.3390/cancers13215529. PMID: 34771691; PMCID: PMC8582907.12. Riechelmann H, Dejaco D, Steinbichler TB, Lettenbichler-Haug A, Anegg M, Ganswindt U, Gamerith G, Riedl D. Functional Outcomes in Head and Neck Cancer Patients. Cancers (Basel). 2022 Apr 25;14(9):2135. doi: 10.3390/cancers14092135. PMID: 35565265; PMCID: PMC9099625.