hypofractionated radiotherapy in elderly/frail head and neck cancer patients: our experience from COVID-19 pandemic.
Purpose/Objective
Head and neck cancer (HNC) remains a significant health concern worldwide. Approximately 50% of HNC occur in the elderly patients and this rate is destined to increase over time, due to the aging of the population. The treatment of HNC poses unique challenges, as it often requires a combination of surgery, chemotherapy, and radiotherapy (RT). Additionally, age-related comorbidities and frailty may complicate the management of HNC in this setting of patients. RT alone has been one of the treatment options for patients with locally advanced HNC squamous cell carcinoma (SCC) with contraindications to chemotherapy, such as cardiac risk, renal or hepatic impairment, frailty or advanced age, and patient choice. In recent years, hypofractionated RT (HFRT) has emerged as an alternative treatment approach, offering the potential to reduce the overall treatment duration while maintaining or even improving treatment outcomes. Several clinical studies have investigated the efficacy and safety of HFRT in HNC. However, robust data are lacking and mainly concern oropharyngeal and laryngeal carcinoma or palliative treatments. The emergence of the COVID-19 pandemic in late 2019 had a profound impact on healthcare systems worldwide. One significant consequence was the need to adapt cancer treatment protocols to minimize patient exposure to the virus while maintaining treatment efficacy. HFRT, with its potential to shorten treatment duration, became an attractive option during this time. The purpose of this study is to report our preliminary retrospective experience on elderly/frail locally advanced HNC patients treated with HFRT, and to assess how the COVID-19 pandemic influenced treatment duration.
Material/Methods
We conducted a retrospective analysis of locally advanced HNC patients aged 70 years and older, not candidate to surgery nor chemotherapy and treated with HFRT alone at our Institution from 2021 to 2022. Gross tumor volume (GTV) was determined according to clinical examination, computed-tomography scan (CT), magnetic resonance imaging (MRI), or positron emission tomography scan (PET). Two clinical target volumes (CTV) were identified (high and low risk). HFRT was delivered with a Linear Accelerator (Trilogy, Varian, Palo Alto, CA, USA) with intensity-modulated (IMRT) or volumetric-modulated (VMAT) RT technique and daily image guidance. HFRT regimens included 60 Gy in 25 fractions over 5 weeks (2.4 Gy per fraction) for CTV-high risk and 50 Gy in 25 fractions over 5 weeks (2.0 Gy per fraction) for CTV-low risk. Patients were evaluated by clinical/endoscopic examination and CT or MRI imaging every 3 months after the completion of HFRT. Response to treatment on imaging (complete or partial response, stable disease), overall survival (OS) and Radiation Therapy Oncology Group (RTOG) Toxicity Criteria were assessed.
Results
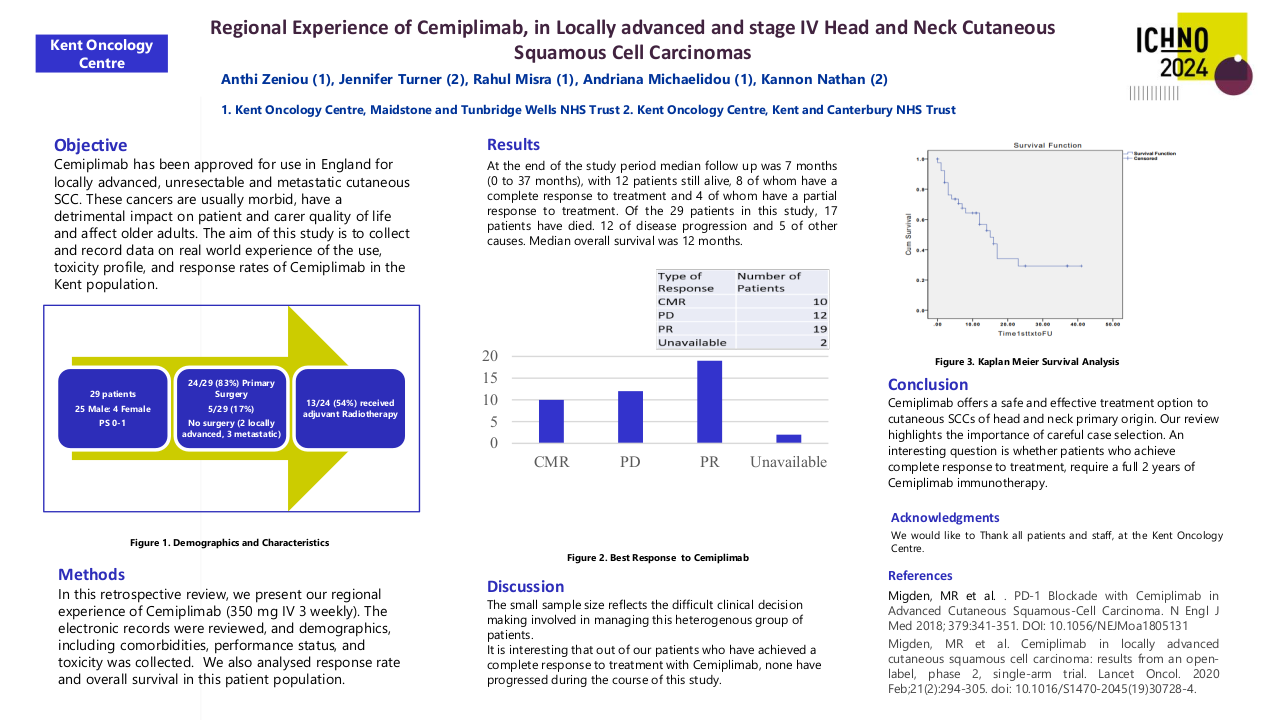
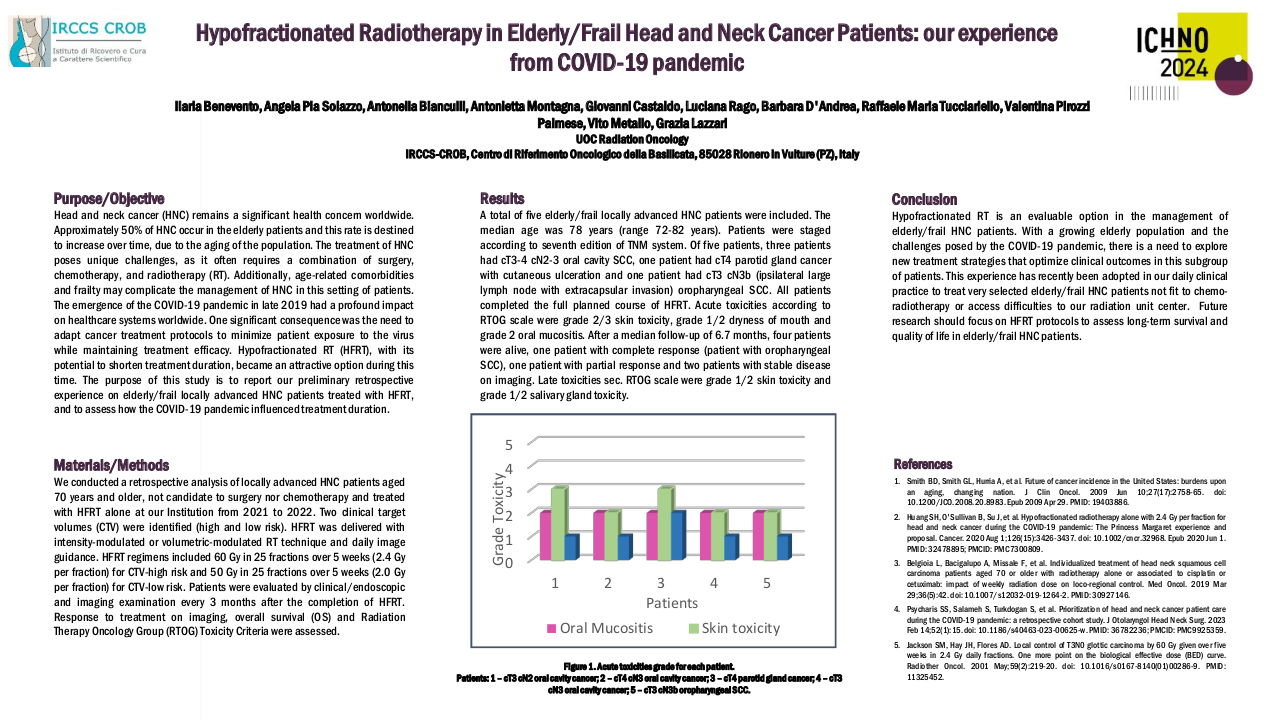
A total of five elderly/frail locally advanced HNC patients were included. The median age was 78 years (range 72-82 years). Patients were staged according to seventh edition of TNM system. Of five patients, three patients had cT3-4 cN2-3 oral cavity SCC, one patient had cT4 parotid gland cancer with cutaneous ulceration and one patient had cT3 cN3b (ipsilateral large lymph node with extracapsular invasion) oropharyngeal SCC. All patients completed the full planned course of HFRT. Acute toxicities according to RTOG scale were grade 2/3 skin toxicity, grade 1/2 dryness of mouth and grade 2 oral mucositis. After a median follow-up of 6.3 months, four patients were alive, one patient with complete response (patient with oropharyngeal SCC), one patient with partial response and two patients with stable disease on imaging. Late toxicities sec. RTOG scale were grade 1/2 skin toxicity and grade 1/2 salivary gland toxicity.
Conclusion
In conclusion, HFRT is an evaluable option in the management of elderly/frail HNC patients. With a growing elderly population and the challenges posed by the COVID-19 pandemic, there is a need to explore new treatment strategies that optimize clinical outcomes in this subgroup of patients. This experience has recently been adopted in our daily clinical practice to treat very selected elderly/frail HNC patients not fit to chemo-radiotherapy or access difficulties to our radiation unit center. Future research should focus on HFRT protocols to assess long-term survival and quality of life in elderly/frail HNC patients.
1. Smith BD, Smith GL, Hurria A, et al. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009 Jun 10;27(17):2758-65. doi: 10.1200/JCO.2008.20.8983. Epub 2009 Apr 29. PMID: 19403886.2. Huang SH, O'Sullivan B, Su J, et al. Hypofractionated radiotherapy alone with 2.4 Gy per fraction for head and neck cancer during the COVID-19 pandemic: The Princess Margaret experience and proposal. Cancer. 2020 Aug 1;126(15):3426-3437. doi: 10.1002/cncr.32968. Epub 2020 Jun 1. PMID: 32478895; PMCID: PMC7300809.3. Belgioia L, Bacigalupo A, Missale F, et al. Individualized treatment of head neck squamous cell carcinoma patients aged 70 or older with radiotherapy alone or associated to cisplatin or cetuximab: impact of weekly radiation dose on loco-regional control. Med Oncol. 2019 Mar 29;36(5):42. doi: 10.1007/s12032-019-1264-2. PMID: 30927146.4. Caudell JJ, Torres-Roca JF, Gillies RJ, et al. The future of personalised radiotherapy for head and neck cancer. Lancet Oncol. 2017 May;18(5):e266-e273. doi: 10.1016/S1470-2045(17)30252-8. Epub 2017 Apr 26. PMID: 28456586; PMCID: PMC7771279.5. Psycharis SS, Salameh S, Turkdogan S, et al. Prioritization of head and neck cancer patient care during the COVID-19 pandemic: a retrospective cohort study. J Otolaryngol Head Neck Surg. 2023 Feb 14;52(1):15. doi: 10.1186/s40463-023-00625-w. PMID: 36782236; PMCID: PMC9925359.6. Prajoko YW, Supit T. Radiotherapy service amidst COVID-19: Experience from Tertiary Referral Hospital in Semarang, Indonesia. J Public Health Res. 2023 Sep 12;12(3):22799036231197189. doi: 10.1177/22799036231197189. PMID: 37711727; PMCID: PMC10498704.7. Jackson SM, Hay JH, Flores AD. Local control of T3N0 glottic carcinoma by 60 Gy given over five weeks in 2.4 Gy daily fractions. One more point on the biological effective dose (BED) curve. Radiother Oncol. 2001 May;59(2):219-20. doi: 10.1016/s0167-8140(01)00286-9. PMID: 11325452.8. Corry J, Peters LJ, Costa ID, et al. The 'QUAD SHOT'--a phase II study of palliative radiotherapy for incurable head and neck cancer. Radiother Oncol. 2005 Nov;77(2):137-42. doi: 10.1016/j.radonc.2005.10.008. Epub 2005 Nov 2. PMID: 16260054.9. Ferris RL, Flamand Y, Weinstein GS, et al. Evaluation of response and quality of life with palliative single-fraction radiation therapy in patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg. 2016;142(10):974-981. doi:10.1001/jamaoto.2016.1674.10. Pfister DG, Spencer S, Brizel DM, et al. Head and Neck Cancers, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18(7):873-898. doi:10.6004/jnccn.2020.0023.