Survival outcomes of elderly patients treated with a curatively-intended treatment for HPV-related oropharyngeal cancer: a multicenter cohort study
Purpose/Objective
The rising incidence of Human Papilloma Virus (HPV) related oropharyngeal squamous cell carcinoma (OPC) in the older population has been confirmed by recent epidemiologic reports. An increase of over 50% is expected in the population aged older than 65 years in the next decade. Some authors have focused their investigations on the “late” elderly subgroup defined as patients (pts) aged 75 years or older, still underrepresented in clinical trials. Indeed, there is a significant lack of data on their disease trajectory. The purpose of our experience was to evaluate the pattern of clinical practice in this specific subgroup of pts within the Italian Association of Radiotherapy and Clinical Oncology (AIRO).
Material/Methods
An observational retrospective study was conducted over a 6-year period (2015-2021). Consecutive patients older than 75 years at diagnosis with a histologically-confirmed HPV positive (p16 immunohistochemistry/HPV DNA-in situ hybridization) OPC eligible for a curatively-intended treatment were included. Overall survival (OS) was defined as the time from OPC diagnosis to last follow-up or death from any cause. Progression-free survival (PFS) was defined as the time from the last day of curative-intended treatment to disease progression or death from any cause. Median OS and PFS was estimated by the Kaplan-Meyer method. A log-rank test was employed to test different variables: smoking history, presence of caregiver, employed treatment modality and age (< or > 80 years) correlated with longer OS. Hazard ratios (HR) for the association between the variables of interest and the risk of death were obtained by univariate Cox regression analysis. A p-value <0.05 was considered statistically significant. Acute toxicity was evaluated according to CTCAE v. 5.0
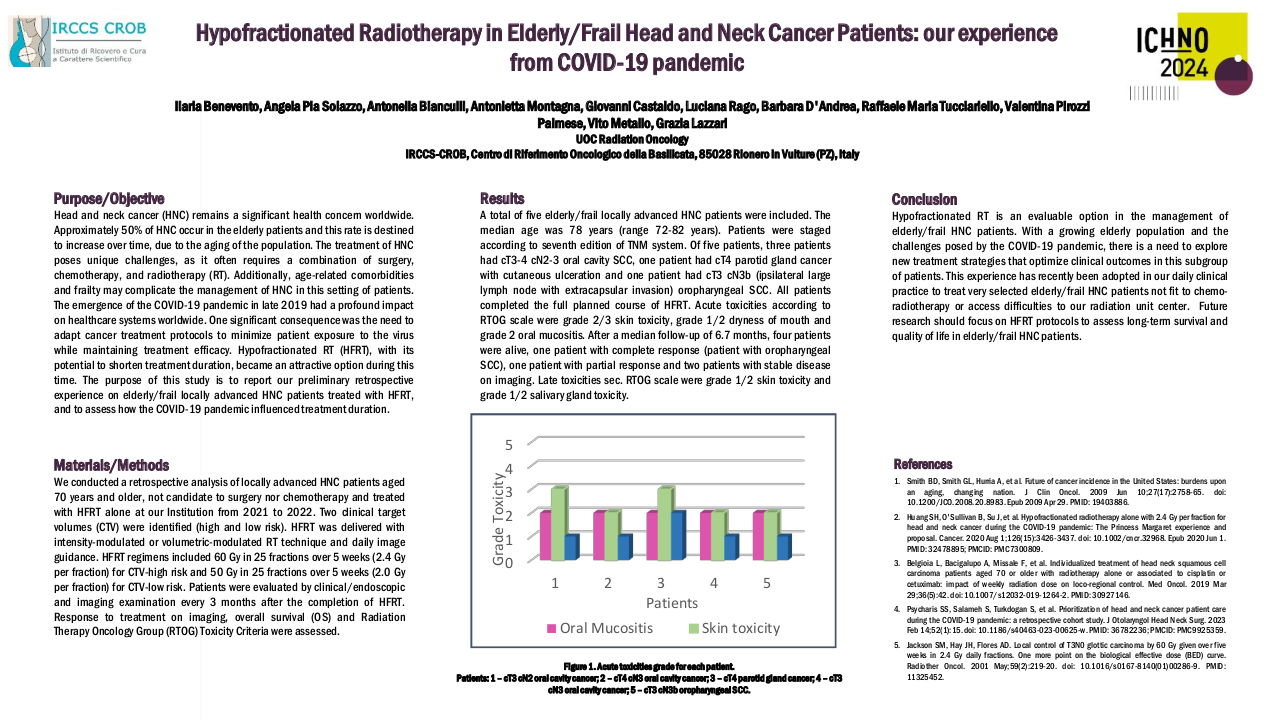
Results
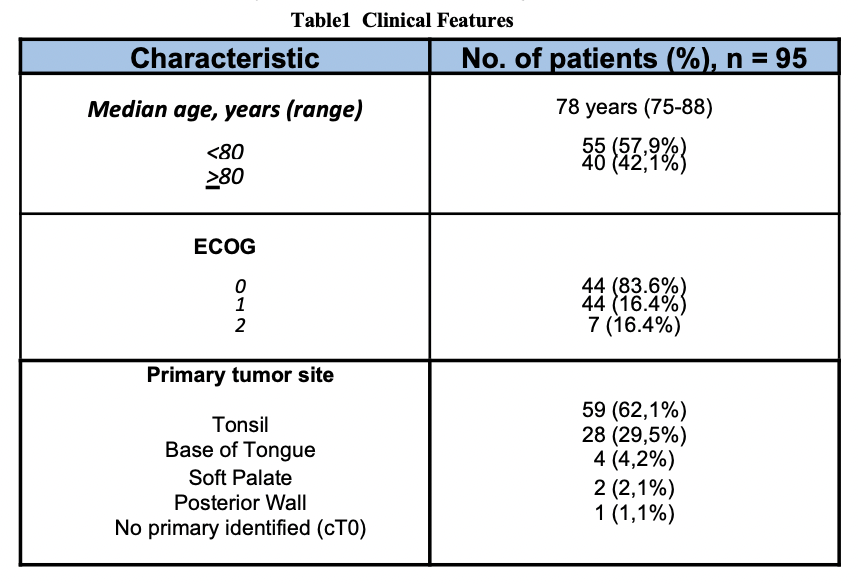
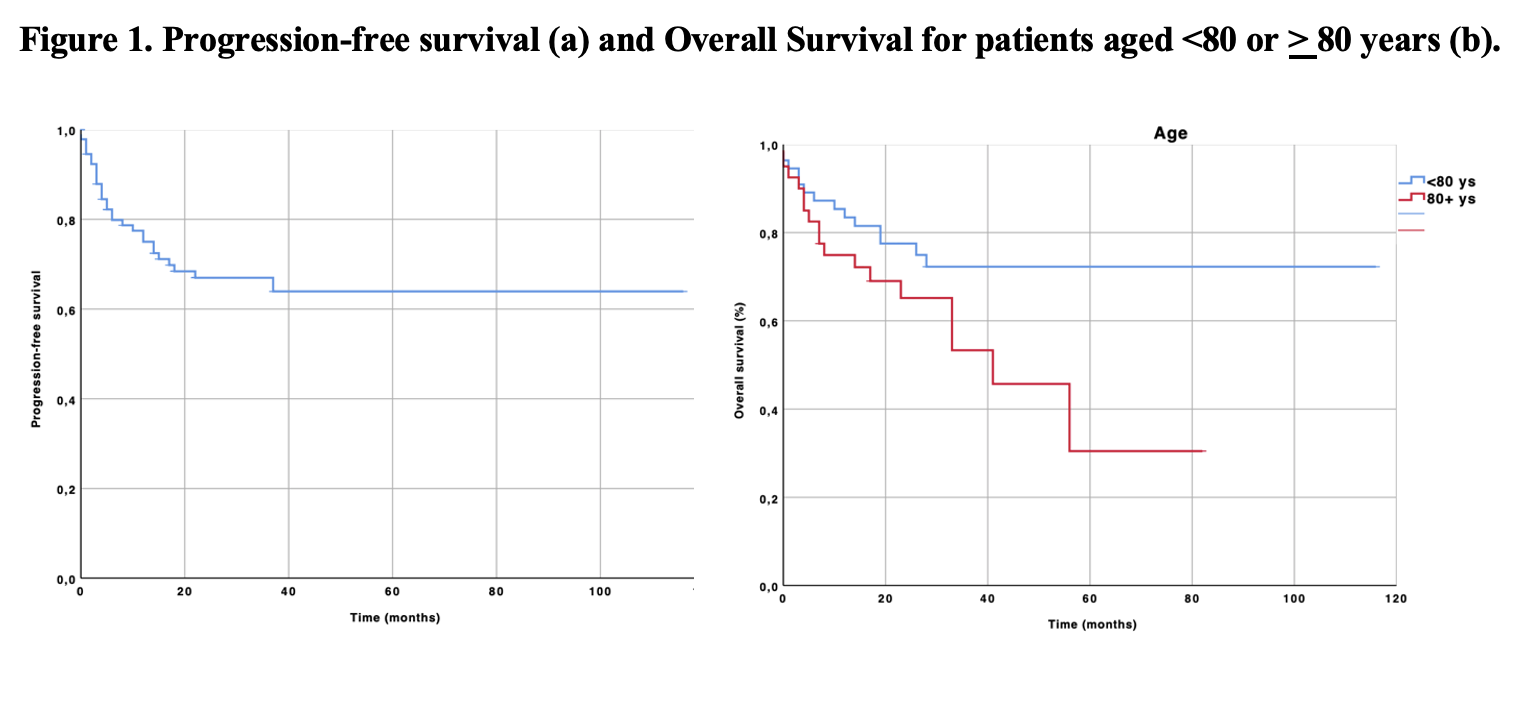
A cohort of 95 pts was included in our analysis. The median age was 78 years (table 1). ECOG PS 0-1 and locally advanced disease were reported for the vast majority of patients, 92.6% and 89.4% (in stage III/IV according to TNM 7thedition) respectively. As expected, exclusive radiotherapy (RT) was the most common adopted strategy. After a median follow- up of 25 months (range: 0-116), 64 patients were alive (67.3%). The one and two-year PFS were 75% and 67%, the median PFS was not reached (Figure 1a). The one and two-year OS rates were 83% and 75%, respectively, whereas the median OS was not reached. Among the tested variables, belonging to the group of age >80 years was associated with a worse OS (p=0.0429; HR for death, 2.15, 95% CI 1.00-4.60, Figure 1b), whereas no impact on survival was associated to the smoking history (p=.011), treatment modality (p=0.32) and presence of caregiver (p=0.65). The toxicity profile was acceptable (>G3 toxicity of 29.4%), although 6 patients (6.3%) died due to potential treatment-related complications. Further analyses on radiation dose, target volumes and pattern of failure will be reported
Conclusion
To the best of our knowledge, our series represents one of the largest to date on “late” elderly population with non-metastatic HPV positive OPC treated with a curatively-intended, RT-based approach. Thanks to the appropriate selection of pts, an optimal survival outcome can be achieved with standard treatment options, in line with data reported for the younger population. Further prospective studies investigating larger series of older pts are warranted in order to confirm our conclusions.