Radiotherapy fraction delivery time does not affect survival outcomes in patients with oropharynx cancer, unselected for chronotype
Purpose/Objective
The rhythmic expression of clock genes generates circadian rhythms that affect cell cycle progression1. As different stages of the cell cycle correlate with sensitivity to radiation, it has been postulated that the time of day that radiotherapy is delivered can influence treatment outcomes2. Prior studies, including randomised trials, suggest that earlier vs later radiotherapy times are associated with superior outcomes, but these are limited by dichotomisation of treatment times, small patient numbers and cohort heterogeneity3,4.
In this study, we aimed to assess the relationship between radiotherapy time and outcomes for a large, contemporary cohort of oropharynx squamous cell carcinoma (OPSCC) treated at a tertiary cancer centre.
Material/Methods
Design: a retrospective review of prospectively-collected data. Eligibility criteria: all newly-diagnosed cases of non-metastatic OPSCC treated with curative-intent (chemo)radiotherapy at The Christie Hospital between 2012 and 2019. Patient-, cancer- and treated-related information was extracted, including the time of day that each radiotherapy fraction was delivered. The average radiotherapy fraction delivery time per patient was calculated and considered as a continuous variable.
Relationships between average fraction delivery time and other variables were assessed. The primary endpoint of interest was overall survival (OS). Progression-free survival (PFS) was a secondary endpoint. Kaplan-Meier plots were created to show estimated OS according to average fraction delivery time quartile. A multivariable Cox Proportional Hazards (PH) model was fitted, adjusting for relevant patient- and cancer-factors, along with average fraction delivery time, the need for hospital transport (% of fractions), distance of patients’ address from the treating centre and the Index of Multiple Deprivation (IMD) decile as a marker of socio-economic deprivation.
Results
32742 fractions of radiotherapy were delivered for 1119 patients. Patient characteristics are shown in the Table.
| Characteristic | N = 1,1291 |
| Age (years) | 59 (52 - 66) |
| Gender | |
| Female | 249 (22%) |
| Male | 870 (78%) |
| ECOG performance status | |
| 0 | 651 (59%) |
| 1 | 334 (30%) |
| 2 | 104 (9.4%) |
| 3 | 23 (2.1%) |
| ACE-27 co-morbidity index | |
| 0 | 492 (44%) |
| 1 | 351 (31%) |
| 2 | 197 (18%) |
| 3 | 75 (6.7%) |
| Weight (kg) | 76 (65 - 89) |
| Body mass index (kg/m2) | 26.0 (22.7 - 29.2) |
| Smoking history | |
| Current | 465 (42%) |
| Ex | 306 (28%) |
| Never | 331 (30%) |
| Distance from radiotherapy centre (km) | 22 (13 - 34) |
| Surgery (yes) | 264 (24%) |
| Tumour stage (TNMv7) | |
| T1 | 201 (18%) |
| T2 | 448 (40%) |
| T3 | 210 (19%) |
| T4a | 221 (20%) |
| T4b | 39 (3.5%) |
| Nodal stage (TNMv7) | |
| N0 | 189 (17%) |
| N1 | 167 (15%) |
| N2a | 97 (8.7%) |
| N2b | 429 (38%) |
| N2c | 198 (18%) |
| N3 | 39 (3.5%) |
| Tumour p16 status | |
| Negative | 234 (25%) |
| Positive | 713 (75%) |
| Not known | 172 (15%) |
| Induction chemotherapy (yes) | 169 (15%) |
| Concurrent chemotherapy (yes) | 507 (45%) |
| Radiotherapy fractionation schedule | |
| 4 weeks | 75 (6.7%) |
| 6 weeks | 1044 (93%) |
Average fraction delivery time did not correlate with patient age or the distance the patient lives from the radiotherapy centre. On average, married patients were treated earlier in the day than single / separated patients (average fraction delivery time 12:30 vs 13:22). Other patients with an earlier average fraction delivery time were those with superior ECOG performance status (ECOG PS 0-1 vs 2-3, 12:53 vs 13:43), less co-morbidity (ACE-27 score 0-1 vs 2-3, 13:02 vs 13:23) or p16-positive disease (p16-positive vs negative, 12:56 vs 13:46).
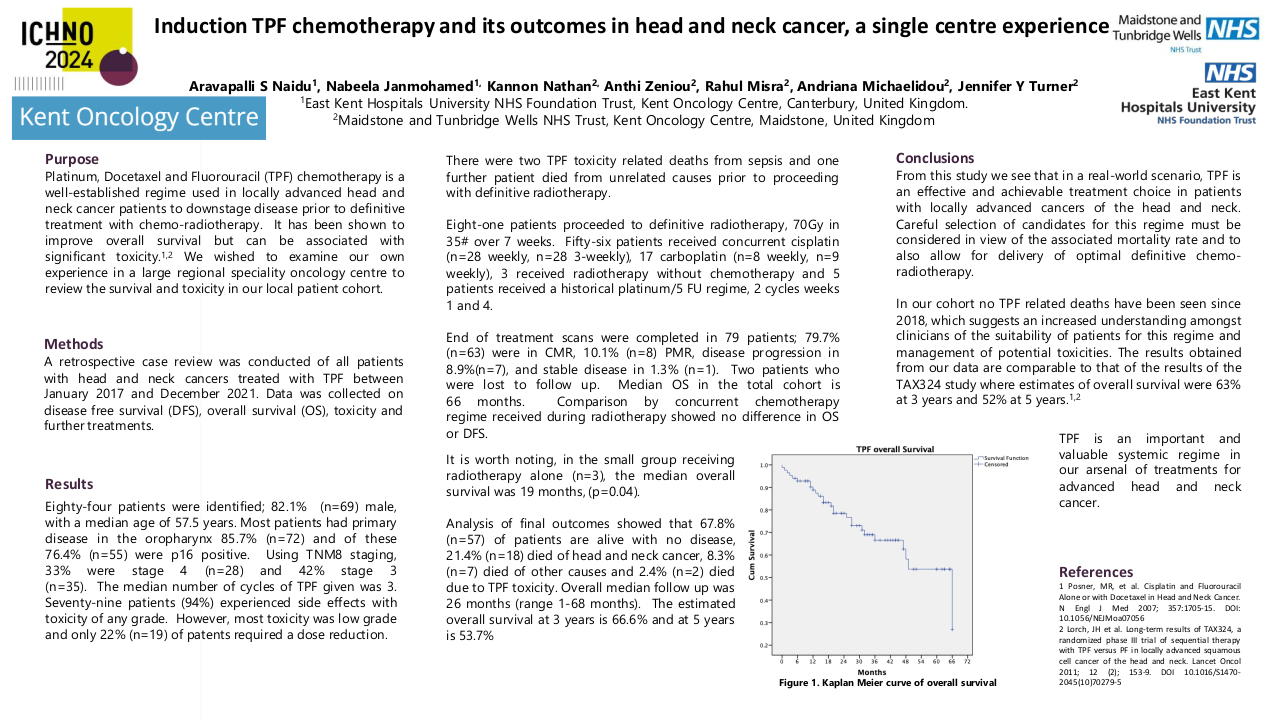
The Figure shows estimated OS according to mean fraction delivery time quartile (quartile 1 = earliest, quartile 4 = latest); mean fraction delivery time quartiles seem to stratify for OS.
On Cox PH regression, when adjusted for relevant patient- (e.g., age, ECOG PS, ACE-27 score, smoking status, IMD decile), cancer- (tumour p16 status, tumour stage, nodal stage) and treatment- factors (radiotherapy fractionation, use of cisplatin chemotherapy) mean fraction delivery time was not prognostic for OS (HR 0.97; 95% CI 0.91 - 1.04; p=0.4) or PFS (HR 1.00; 95% CI 0.93 - 1.07; p>0.9).
Conclusion
When assessing mean fraction delivery time as a continuous variable and adjusting for relevant factors, mean fraction delivery time is not prognostic for patients with OPSCC treated with radical (chemo)radiotherapy. Observations of improved outcomes for patients treated earlier in the day (prior to adjusting for covariates) can be explained by such patients typically being fitter, having less co-morbidity and being more likely to have p16-positive disease.
There is no evidence that circadian rhythm affects survival outcomes in patients with OPSCC, unselected for chronotype.
1. Farshadi, E., Van Der Horst, G. T. J. & Chaves, I. Molecular Links between the Circadian Clock and the Cell Cycle. Journal of Molecular Biology 432, 3515–3524 (2020).2. Harper, E. & Talbot, C. J. Is it Time to Change Radiotherapy: The Dawning of Chronoradiotherapy? Clinical Oncology 31, 326–335 (2019).3. Jiang, D. et al. Does Time of Daily Treatment Matter in Radiation Therapy for Head and Neck Cancer? International Journal of Radiation Oncology*Biology*Physics 93, E348 (2015).4. Elicin, O. et al. The prognostic impact of daytime and seasonality of radiotherapy on head and neck cancer. Radiotherapy and Oncology 158, 293–299 (2021).