Videofluoroscopy assessment of swallowing following dysphagia-optimised IMRT in head and neck cancer
Purpose/Objective
Primary (chemo) radiotherapy (CRT) for head and neck cancers may have an adverse effect on patients’ swallowing function. Minimising RT dose to critical swallowing structures using dysphagia-optimised intensity-modulated RT (DO-IMRT) has been shown to improve post-treatment patient-reported swallowing outcomes. Following the implementation of DO-IMRT as standard of care at our centre for HNC patients treated with primary (C)RT, videofluoroscopy (VFS) as a core monitoring component was piloted for an initial cohort of 30 patients. We present swallowing outcomes based on prospectively collected pre- and post-treatment VFS assessment.
Material/Methods
30 consecutive patients treated with DO-IMRT between March and August 2022 were included. All patients received a radical RT dose of 65 Gy/30 fractions/6 weeks to the tumour and involved nodes, and a prophylactic dose of 54 Gy/30 fractions/6 weeks to regions at risk of microscopic disease – with or without chemotherapy. VFS was performed at baseline and three months following completion of treatment. Analysis of VFS imaging included 1) quantification of depth and response to airway compromise using Penetration-Aspiration Scale (PAS: 1-2 normal, 3-5 penetration, 6-8 aspiration); 2) grading severity of dysphagia with Dynamic Imaging Grade of Swallowing Toxicity (DIGEST: 5-point scale; 0 normal, 4 life-threatening); 3) pathophysiological assessment of swallow using the Modified Barium Swallowing Impairment Profile (MBSImP). PAS was dichotomised in two ways, one to indicate any laryngeal penetration or aspiration (PAS <3 vs PAS ≥3) and one to indicate aspiration not ejected (PAS <7 vs PAS 7-8). For DIGEST and MBSImP, parameters were dichotomised to differentiate normal swallow to mild impairment from moderate-severe impairment (0-1 vs 2+). Dichotomised parameters were compared using McNemar’s test. No corrections for multiplicity were made. PAS and DIGEST were scored by two speech and language therapists (SLTs) independently. MBSImP was scored by one certified SLT who was blinded to diagnosis and clinical assessment outcomes as well as baseline results at time of scoring post-treatment VFS.
Results
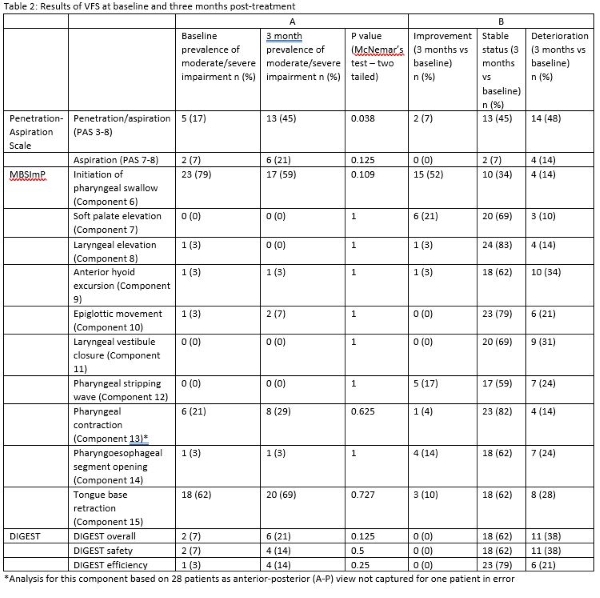
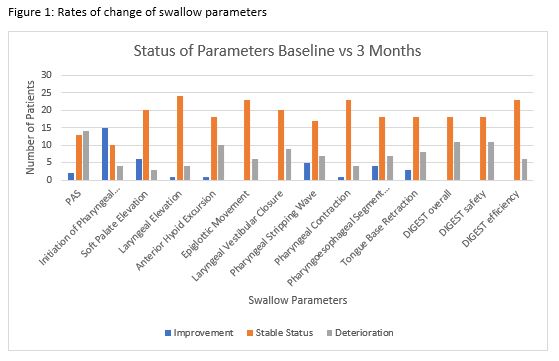
Patient, disease and treatment characteristics are presented in Table 1. One patient died before completion of the post-treatment VFS, therefore final analyses were based on complete data for 29 patients. There was no significant increase in the rates of aspiration not ejected (PAS 7-8) following treatment (p = 0.125), though the prevalence of laryngeal penetration/aspiration (PAS 3-8) increased from 17% at baseline to 45% at three months following treatment completion (p = 0.038) (Table 2:A). 7% of patients had baseline moderate-severe dysphagia as per DIGEST; this increased to 21% following treatment and was not statistically significant (p =0.125) (Table 2:A). All DIGEST scores and subscores remained predominantly stable following treatment. (Table 2:B; Figure 1). There was no statistically significant increase in prevalence of moderate-severe impairment for any analysed MBSImP components of swallowing between pre- and post-treatment VFS (Table 2:A); the most frequent outcome for 9 out of 10 MBSImP components was stability, while initiation of swallow (MBSImP component 6) most frequently showed improvement (Table 2:B; Figure 1).
Table 1: Patient, disease and treatment characteristics
| Characteristics | n (%) |
| Sex | |
| Male | 26 (87) |
| Female | 4 (13) |
| Age at diagnosis | |
| Range 39-74 years | |
| Mean 61 years | |
| Smoking status | |
| Current | 3 (10) |
| Previous | 21 (70) |
| Never | 6 (20) |
| Smoking history | |
| Never | 6 (20) |
| <10 pack years | 5 (17) |
| >10 pack years | 19 (63) |
| Tumour staging | |
| T1 | 4 (13) |
| T2 | 6 (20) |
| T3 | 9 (30) |
| T4 | 11 (37) |
| Nodal staging | |
| N0 | 13 (43) |
| N+ | 17 (57) |
| Disease stage (AJCC 7th edition) | |
| I | 1 (3) |
| II | 5 (17) |
| III | 6 (20) |
| IV | 18 (60) |
| Primary site | |
| Nasopharynx | 2 (7) |
| Oropharynx | 16 (53) |
| - Oropharynx HPV+ | 10 (33 of total) |
| - Oropharynx HPV- | 6 (20 of total) |
| Larynx | 7 (23) |
| Hypopharynx | 5 (17) |
| Treatment | |
| RT | 7 (23) |
| CRT | 20 (67) |
| Induction chemotherapy + CRT | 3 (10) |
| RT neck treatment | |
| Unilateral neck | 1 (3) |
| Bilateral neck | 29 (97) |
| VFS assessment | |
| Baseline | 30 (100) |
| 3 months post-treatment | 29 (97) |
Conclusion
In this small pilot cohort, prospective instrumental evaluation of swallowing function using validated assessment tools showed that functional outcomes following DO-IMRT did not significantly deteriorate at three months post-treatment in comparison to baseline and supports the implementation of this toxicity-sparing RT delivery technique. The prevalence of laryngeal penetration/aspiration (PAS 3-8) did increase statistically significantly over time, but rates of aspiration not ejected (PAS 7-8) specifically did not, which may be of more pertinent clinical importance. Further longitudinal assessment with a larger cohort is required to determine the longer-term benefits of DO-IMRT.
1. Nutting C, Finneran L, Roe J, Sydenham MA, Beasley M, Bhide S, et al. Dysphagia-optimised intensity-modulated radiotherapy versus standard intensity-modulated radiotherapy in patients with head and neck cancer (DARS): a phase 3, multicentre, randomised, controlled trial. The Lancet Oncology [Internet]. 2023 [cited 2023 Aug 15];24(8):868–80. Available from: https://linkinghub.elsevier.com/retrieve/pii/S14702045230026562. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia [Internet]. 1996 Mar 1 [cited 2023 Oct 9];11(2):93–8. Available from: https://doi.org/10.1007/BF004178973. Hutcheson KA, Barrow MP, Barringer DA, Knott JK, Lin HY, Weber RS, et al. Dynamic Imaging Grade of Swallowing Toxicity (DIGEST): Scale development and validation. Cancer [Internet]. 2017 [cited 2023 Oct 9];123(1):62–70. Available from: https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.302834. Hutcheson KA, Barbon CEA, Alvarez CP, Warneke CL. Refining measurement of swallowing safety in the Dynamic Imaging Grade of Swallowing Toxicity (DIGEST) criteria: Validation of DIGEST version 2. Cancer [Internet]. 2022 [cited 2023 Oct 9];128(7):1458–66. Available from: https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.340795. Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, et al. MBS Measurement Tool for Swallow Impairment—MBSImp: Establishing a Standard. Dysphagia [Internet]. 2008 [cited 2023 Oct 9];23(4):392–405. Available from: http://link.springer.com/10.1007/s00455-008-9185-96. Gawryszuk A, Bijl HP, Van Der Schaaf A, Perdok N, Wedman J, Verdonck-de Leeuw IM, et al. Relationship between videofluoroscopic and subjective (physician- and patient- rated) assessment of late swallowing dysfunction after (chemo) radiation: Results of a prospective observational study. Radiotherapy and Oncology [Internet]. 2021 [cited 2023 Jun 16];164:253–60. Available from: https://linkinghub.elsevier.com/retrieve/pii/S01678140210674027. Barbon CEA, Yao CMKL, Alvarez CP, Goepfert RP, Fuller CD, Lai SY, et al. Dysphagia profiles after primary transoral robotic surgery or radiation for oropharyngeal cancer: A registry analysis. Head & Neck [Internet]. 2021 [cited 2023 Aug 15];43(10):2883–95. Available from: https://onlinelibrary.wiley.com/doi/10.1002/hed.26768