Oral microbiome’s impact on mucositis and locoregional tumor control in HNSCC patients undergoing radiotherapy
Purpose/Objective
Recent studies have shown a potential function of the gut microbiome in the immunological modulation of anti-cancer treatments. However, the role of the oral microbiome in head-and-neck squamous cell carcinoma (HNSCC) patients undergoing radiotherapy in terms of radiation-induced toxicities as well as tumor response is largely unknown. Here, we examined a potential influence of the oral microbiome composition on acute radiation-induced mucositis and locoregional tumor control (LRC).
Material/Methods
Saliva samples of two independent prospective trials (SALIVA and ZiSStrans trial [DRKS00012947]), in which HNSCC patients undergoing (chemo)radiation were enrolled, were analyzed in terms of their oral microbiome composition. In both trials, unstimulated saliva was collected before the first radiotherapy application and stored at -80°C. Baseline oral microbiome was examined using V3-4 16S rRNA sequencing, and bioinformatic analyses were carried out in R (v4.3.1). Kaplan-Meier analyses were carried out regarding LRC.
Results
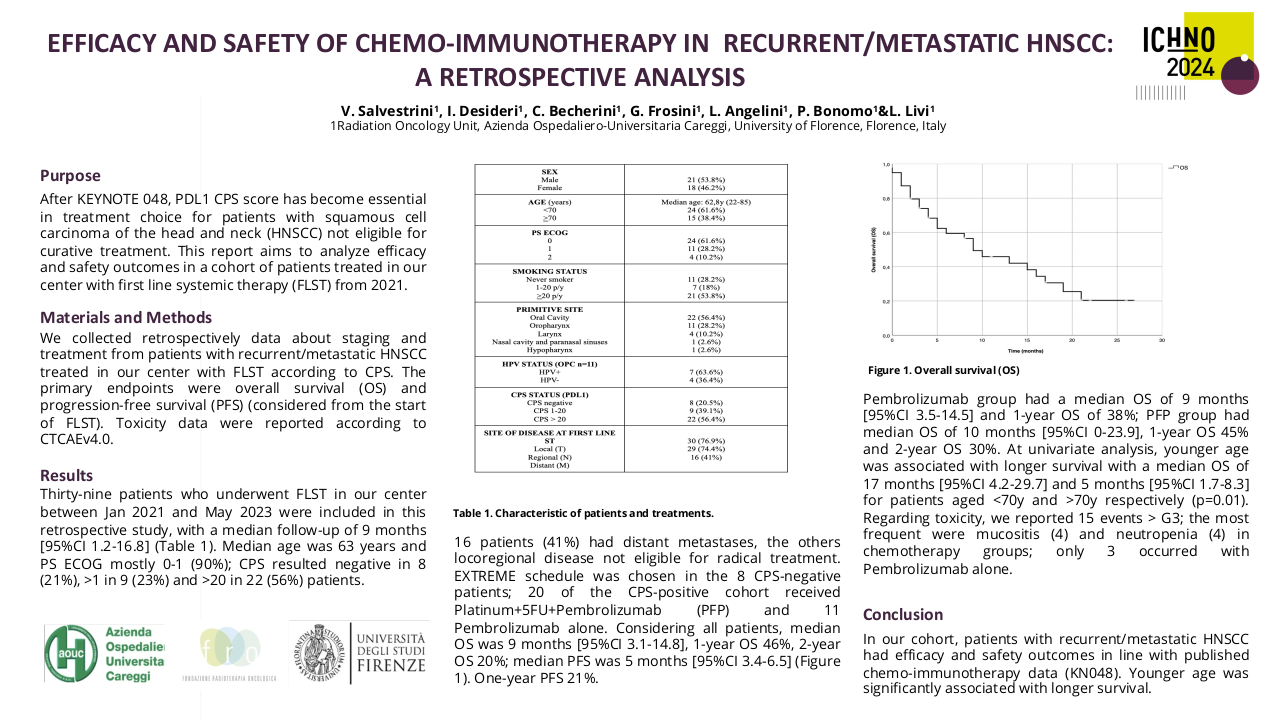
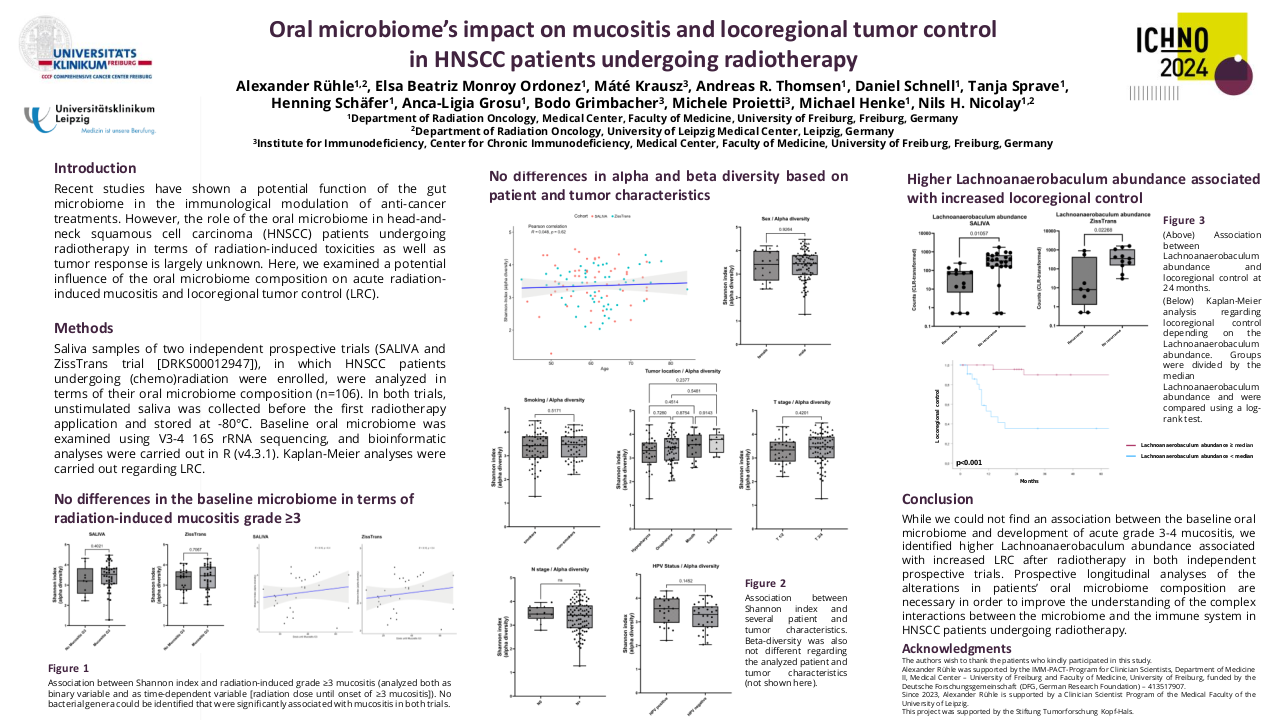
A total of 106 HNSCC patients (53 in the SALIVA trial, 53 in the ZiSStrans trial), who were treated with definitive (chemo)radiation, had stored saliva samples available and could be analyzed. Median age was 60 years (SALIVA) and 61 years (ZiSStrans), most common tumor localization was the oropharynx (n=25 in both trials), and majority of patients had a positive smoking history (n=29 [SALIVA], n=27 [ZiSStrans]). Fourty-four (83%) and 30 (57%) patients in the SALIVA and ZiSStrans trial developed acute grade 3-4 mucositis during treatment, respectively. Grade 3-4 mucositis occurred after a median radiation dose of 34 Gy (SALIVA) and 31.5 Gy (ZiSStrans). 2-year LRC rate was 69% and 72% in the SALIVA and ZiSStrans trial, respectively. No differences in alpha diversity were found in terms of patient age, sex, T stage, N stage, tumor localization and smoking status in both trials (p>0.05), neither did the beta diversity analysis reveal relevant differences between these groups. Furthermore, neither alpha nor beta diversity was associated with development of grade 3-4 mucositis in the two trials (p>0.05). In the ZiSStrans trial, Shannon index was significantly higher in patients with no locoregional recurrence after 2 years (p=.03), which was not validated in the SALIVA trial (p=0.35). Lower Lachnoanaerobaculum abundance (p=0.02 [SALIVA], p=0.03 [ZiSStrans], ALDEx2, Wilcoxon-test) were associated with increased 2-year locoregional recurrence rates in both the SALIVA and ZissTrans trial. 2-year LRC was 96% (SALIVA) and 85% (ZiSStrans) in patients with Lachnoanaerobaculum abundance above the median value versus 35% (SALIVA) and 58% (ZiSStrans) in patients with Lachnoanaerobaculum abundance below the median (p<0.05, log-rank).
Conclusion
While we could not find an association between the baseline oral microbiome and development of acute grade 3-4 mucositis, we identified higher Lachnoanaerobaculum abundance associated with increased LRC after radiotherapy in both independent prospective trials. In terms of oral mucositis, further in-depth analyses of the oral microbiome composition in both prospective trials are ongoing to examine potential associations between distinct bacterial genera and the onset of grade 3-4 mucositis. Prospective longitudinal analyses of the alterations in patients’ oral microbiome composition are necessary in order to improve the understanding of the complex interactions between the microbiome and the immune system in patients with HNSCC undergoing radiotherapy.