Is adjuvant radiotherapy necessary for early-stage oral cavity cancer patients with the worst pattern of invasion-V?
Purpose/Objective
We aimed to investigate the impact of the worst pattern of invasion (WPOI-V), an indicator of biological aggressiveness, on survival outcomes, as well as the potential need for adjuvant radiotherapy in squamous cell oral cavity cancers.
Material/Methods
A total of 162 patients who underwent surgical procedures at our center between 2017 and 2023 were included in the study. The median age of the patients was 65 years (range, 18-91 years). Tumor locations encompassed the lip (n=60), tongue (n=49), gingiva and buccal mucosa (n=23), and other sites (n=30). Patients were categorized into two groups: those with early-stage disease (T1-2 or N0) (n=80) and those with locally advanced disease (T3-4 or N+) (n=82). Cancer-specific survival (CSS) was defined as the time to local, regional, or systemic progression, while overall survival (OS) was defined as the time to death from any cause following the date of surgery. The Kaplan-Meier method was employed for survival analysis, and statistical significance was set at p<0.05.
Results
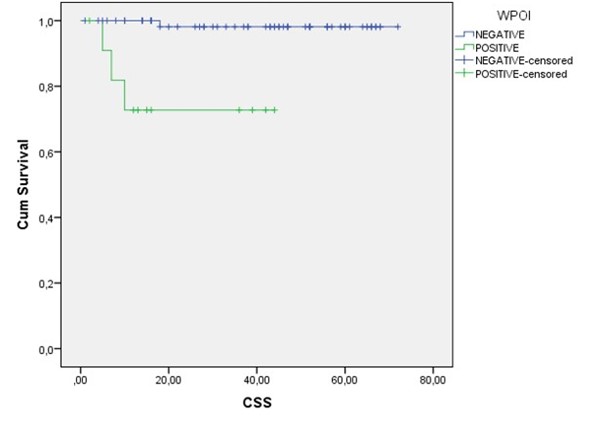
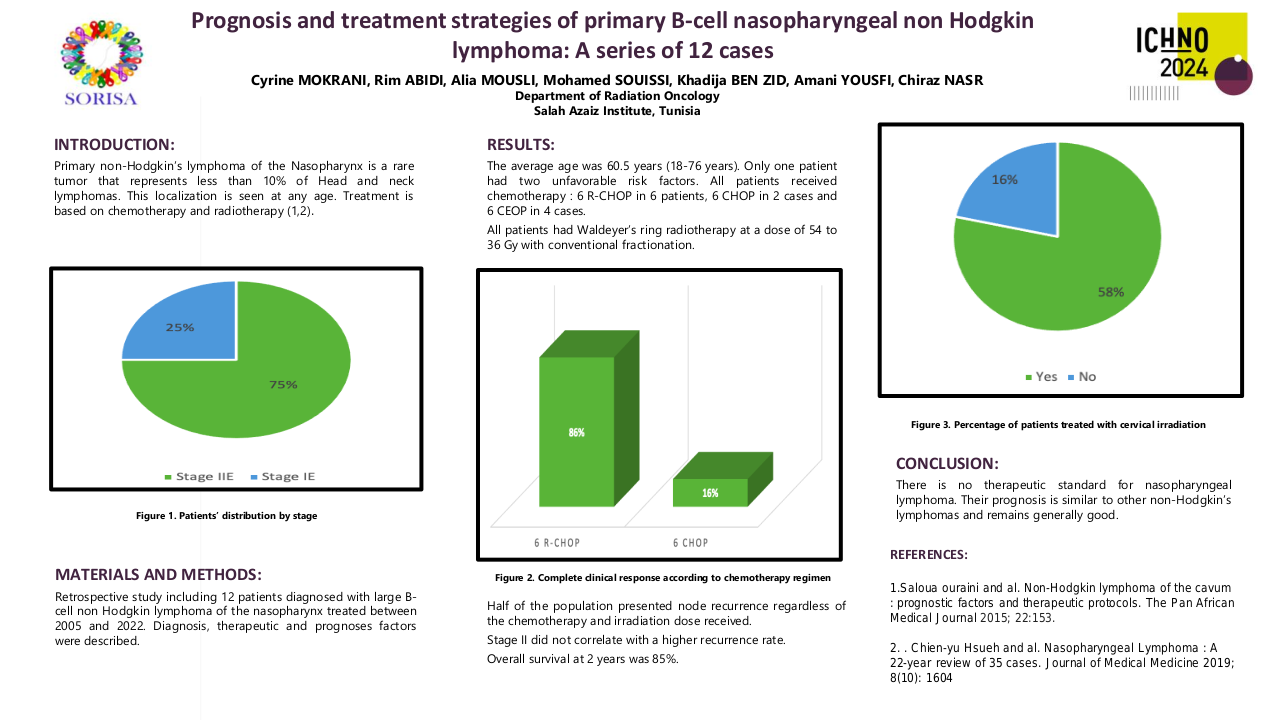
The median follow-up duration was 36 months, with a range from 0 to 72 months. Local, regional, and/or systemic progression was observed in 26 patients, resulting in distant metastasis in 13 cases, local regional relapse in 8 cases, and second primary lung cancer in 2 cases. The three-year Cancer-Specific Survival (CSS) was significantly worse in patients with the presence of WPOI-V (63% vs. 86.9%, p=0.000) (see Figure 1). The difference was notably more pronounced in early-stage or younger patients. In multivariate analysis, the only significant factor influencing CSS in the early stage was WPOI-V (p=0.008) (Figure 1).There was no significant difference observed in OS.
Conclusion
The presence of WPOI-V in both early-stage and locally advanced patients serves as an indicator of a poor prognosis. This finding may represent a novel factor that warrants consideration for the inclusion of adjuvant therapy in the treatment of early-stage patients.
•Brandwein-Gensler M, Teixeira MS, Lewis CM, Lee B, Rolnitzky L, Hille JJ, Genden E, Urken ML, Wang BY. Oral squamous cell carcinoma: histologic risk assessment, but not margin status, is strongly predictive of local disease-free and overall survival. Am J Surg Pathol. 2005 Feb;29(2):167-78. doi: 10.1097/01.pas.0000149687.90710.21. PMID: 15644773.•Tan A, Taskin T. Tumor Budding Should Be in Oral Cavity Cancer Reporting: A Retrospective Cohort Study Based on Tumor Microenvironment. Cancers (Basel). 2023 Aug 1;15(15):3905. doi: 10.3390/cancers15153905. PMID: 37568721; PMCID: PMC10416929.•Fonseca D, Khemani R, Pasam MK, Tagore R, Rao BV, Kodandapani S, Rao C, V N Raju KV, Rao TS. Histological risk score and its role in predicting recurrence in early-stage oral squamous cell carcinomas. Indian J Pathol Microbiol. 2023 Jul-Sep;66(3):444-448. doi: 10.4103/ijpm.ijpm_514_21. PMID: 37530322.•Kopecká K, Pink R. Pattern of invasion of oral squamous cell carcinoma and its relation to the presence of nodal metastases - a review. Acta Chir Plast. 2023 Spring;65(1):28-33. English. doi: 10.48095/ccachp202328. PMID: 37211421.•Lakhera KK, Nama Y, Maan P, Jindal R, Patel P, Singh S, Hussain A, Sharma RG. Worst Pattern of Invasion as a Predictor of Nodal Metastasis in Early-Stage Oral Squamous Cell Carcinoma. Indian J Surg Oncol. 2023 Mar;14(1):160-168. doi: 10.1007/s13193-022-01639-y. Epub 2022 Sep 10. PMID: 36891424; PMCID: PMC9986178.