Pre-operative Radiotherapy for Sinonasal Squamous Cell Carcinoma: outcomes and patient selection
Purpose/Objective
Resectable sinonasal squamous cell carcinoma (SNSCC) is often managed by surgery +/- post-operative radiation (postop-RT), guided by surgical pathology. In our institution, pre-operative radiation (preop-RT) +/- chemotherapy has been used in select cases after multidisciplinary input from radiation, surgical, and medical oncology teams. Preop-RT has the advantages of lower dose and smaller/better defined volumes in non-surgically perturbed tissues, which can be especially important for treatment approximating optic structures. The aim of this study is to evaluate preop-RT, compared to standard postop-RT, in patients with SNSCC, focusing on oncologic outcomes and patient selection.
Material/Methods
All newly diagnosed SNSCC treated with preop-RT or postop-RT from 2005 to 2021 were included. Clinical characteristics and outcomes were compared between preop-RT vs postop-RT cohorts. Outcome endpoints included overall survival (OS), disease-free survival (DFS), locoregional control (LRC) and distant control (DC). OS and DFS were estimated with Kaplan-Meier method while LRC and DC were calculated with competing risk methods.
Results
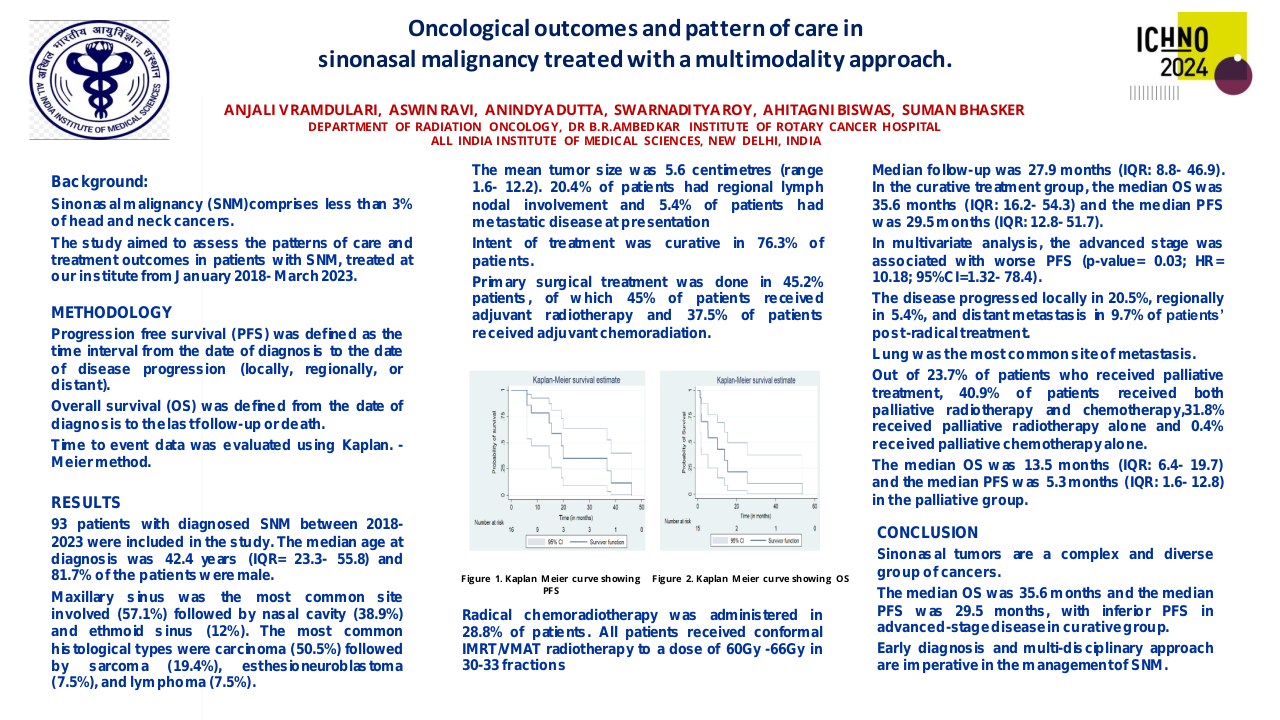
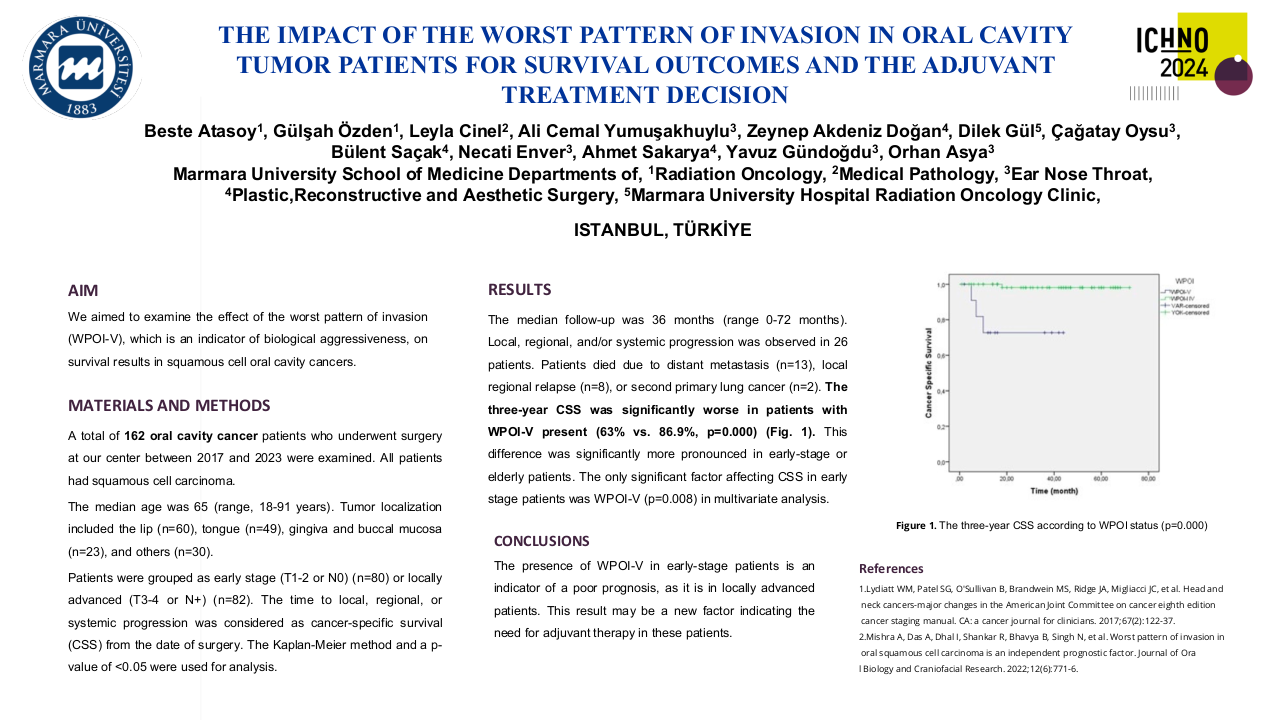
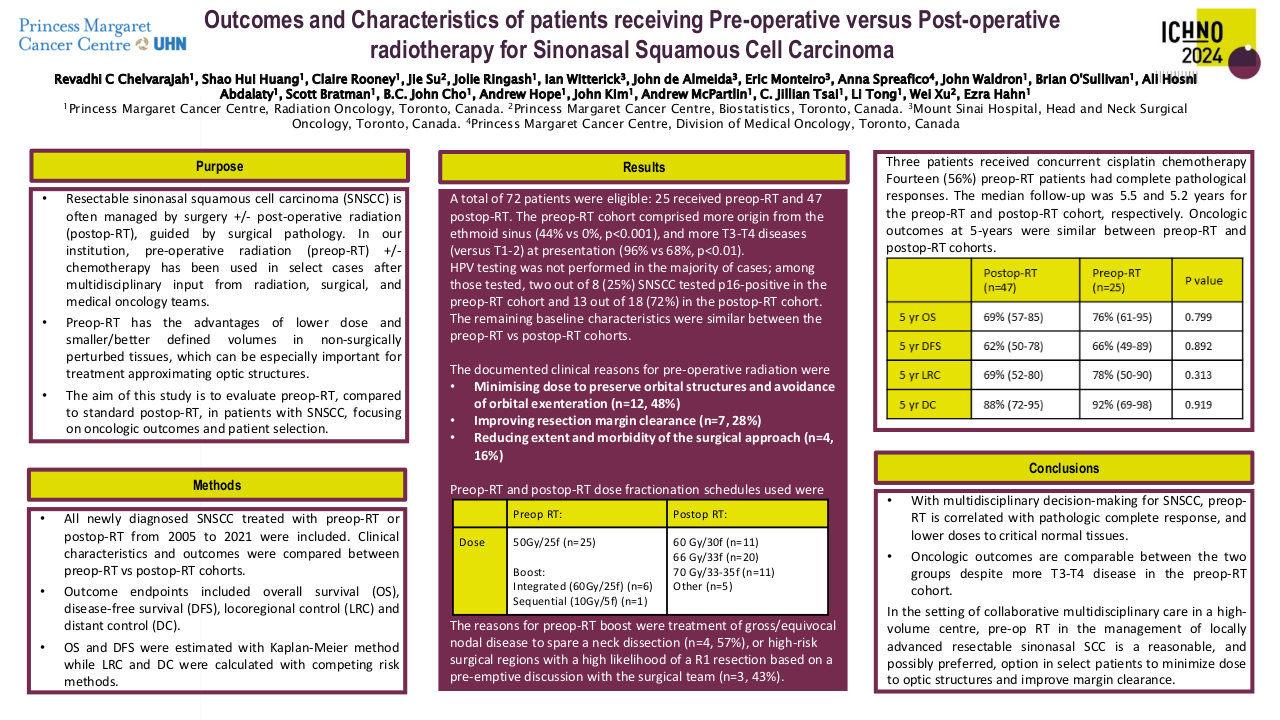
A total of 72 patients were eligible: 25 received preop-RT and 47 postop-RT. The preop-RT cohort comprised more origin from the ethmoid sinus (44% vs 0%, p<0.001), and more T3-T4 diseases (versus T1-2) at presentation (96% vs 68%, p<0.01). HPV testing was not performed in the majority of cases; among those tested, two out of 8 (25%) SNSCC tested p16-positive in the preop-RT cohort and 13 out of 18 (72%) in the postop-RT cohort. The remaining baseline characteristics were similar between the preop-RT vs postop-RT cohorts. The documented clinical reasons for pre-operative radiation included minimizing dose to preserve orbital structures and avoidance of orbital exenteration (n=12, 48%), improving resection margin clearance (n=7, 28%), and reducing extent and morbidity of the surgical approach (n=4, 16%). All patients in preop-RT cohort received 50 Gy in 25 fractions (50 Gy/25f) to the primary site, with 7 patients receiving a boost to 60 Gy (6 patients with simultaneous integrated boost, 1 patient with sequential 10 Gy/5f boost). The reasons for boost were treatment of gross/equivocal nodal disease to spare a neck dissection (n=4, 57%), or high-risk surgical regions with a high likelihood of a R1 resection based on a pre-emptive discussion with the surgical team (n=3, 43%). Three patients received concurrent cisplatin chemotherapy. Patients in the postop-RT cohort received 60 Gy/30f (n=11), 66 Gy/33f (n=20), 70 Gy/33-35f (n=11), and other (n=5). Fourteen (56%) preop-RT patients had complete pathological responses. The median follow-up was 5.5 and 5.2 years for the preop-RT and postop-RT cohort, respectively. Oncologic outcomes at 5-years were similar between preop-RT and postop-RT cohorts: OS 76% vs 69% (p=0.799), DFS 66% vs 62% (p=0.892), LRC 78% vs 69% (p=0.313), and DC 92% vs 88% (p=0.919), respectively (Table 1).
Table 1. Oncologic Outcomes
|
|
Postop-RT (n=47) |
Preop-RT (n=25) |
P value |
|
5-year Outcomes |
|
|
|
|
OS |
69% (57-85) |
76% (61-95) |
0.799 |
|
DFS |
62% (50-78) |
66% (49-89) |
0.892 |
|
LRC |
69% (52-80) |
78% (50-90) |
0.313 |
|
DC |
88% (72-95) |
92% (69-98) |
0.919 |
Conclusion
With multidisciplinary decision-making for SNSCC, preop-RT is correlated with pathologic complete response, and lower doses to critical normal tissues. Oncologic outcomes are comparable between the two groups despite more T3-T4 disease in the preop-RT cohort. In the setting of collaborative multidisciplinary care in a high-volume centre, pre-op RT in the management of locally advanced resectable sinonasal SCC is a reasonable, and possibly preferred, option in select patients to minimize dose to optic structures and improve margin clearance.