Oncological outcomes and pattern of care in sinonasal malignancy treated with a multimodality approach.
Purpose/Objective
The study aimed to assess the patterns of care and treatment outcomes in patients with sinonasal malignancy (SNM), treated at our institute from January 2018- March 2023.
Material/Methods
Patients with biopsy proven SNM were included in this retrospective analysis. Progression free survival (PFS) was defined as the time interval from the date of diagnosis to the date of disease progression (locally, regionally, or distant). Overall survival (OS) was defined from the date of diagnosis to the last follow-up or death. Univariate Cox regression analysis was done to evaluate the relationship between treatment factors and survival outcomes. Time to event data was evaluated using Kaplan. -Meier method.
Results
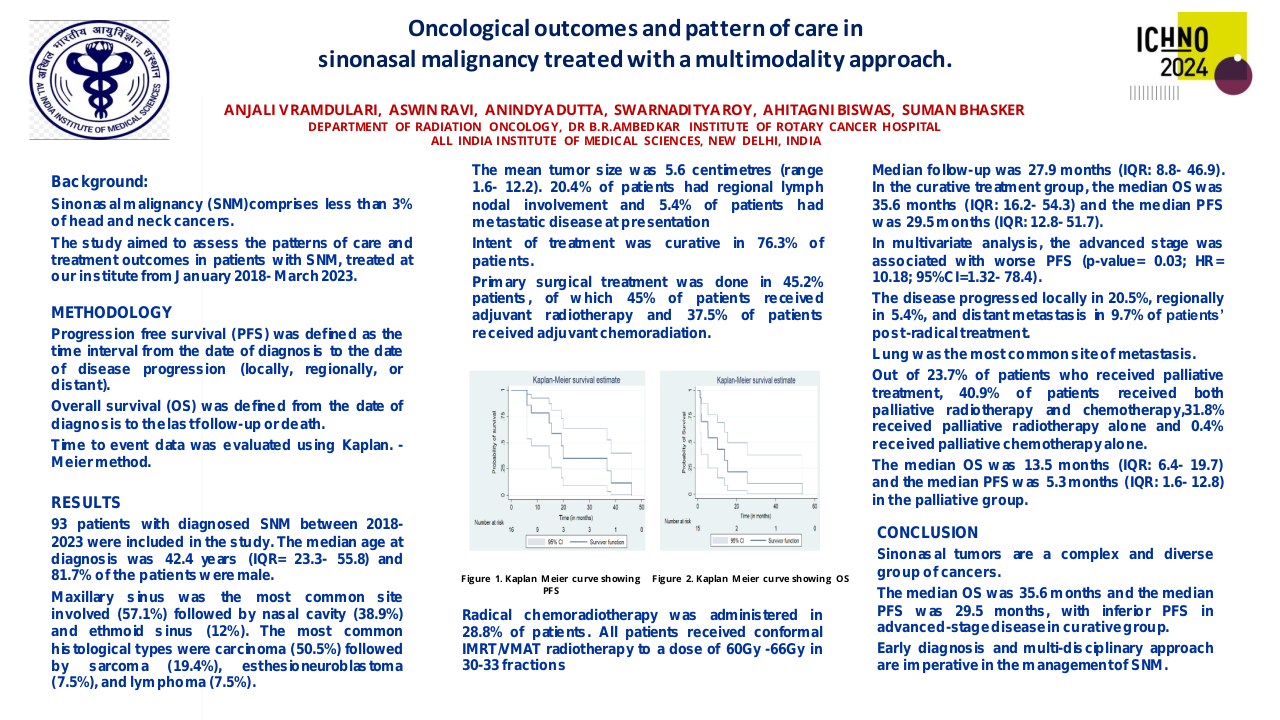
A total of 93 patients with diagnosed SNM between 2018-2023 were included in the study. The median age at diagnosis was 42.4 years (IQR= 23.3- 55.8). 81.7% of the patients were male. Maxillary sinus was the most common site involved (57.1%) followed by nasal cavity (38.9%) and ethmoid sinus (12%). The most common histological types were carcinoma (50.5%) followed by sarcoma (19.4%), esthesioneuroblastoma (7.5%), and lymphoma (7.5%). Among carcinoma, squamous cell carcinoma (61.6%) was the most common subtype followed by adenoid cystic carcinoma. The mean tumor size was 5.6 centimetres (range 1.6- 12.2). 20.4% of patients had regional lymph nodal involvement and 5.4% of patients had metastatic disease at presentation. Intent of treatment was curative in 76.3% of patients. Primary surgical treatment was done in 45.2% patients, of which 45% of patients received adjuvant radiotherapy and 37.5% of patients received adjuvant chemoradiation. Radical chemoradiotherapy was administered in 28.8% of patients. All patients received conformal IMRT/VMAT radiotherapy to a dose of 60Gy -66Gy in 30-33 fractions. Median follow-up was 27.9 months (IQR: 8.8- 46.9). In the curative treatment group, the median OS was 35.6 months (IQR: 16.2- 54.3) and the median PFS was 29.5 months (IQR: 12.8- 51.7). In univariate analysis, patients who did not complete the planned treatment were associated with decreased OS (p-value= 0.03; HR= 5.57; 95%CI= 1.21- 25.57), advanced-stage disease was associated with inferior PFS (p- value= 0.026; HR= 9.81; 95%CI=1.29- 74.44). In multivariate analysis, the advanced stage was associated with worse PFS (p-value= 0.03; HR= 10.18; 95%CI=1.32- 78.4). The disease progressed locally in 20.5%, regionally in 5.4%, and distant metastasis in 9.7% of patients’ post-radical treatment. Lung was the most common site of metastasis. Out of 23.7% of patients who received palliative treatment, 40.9% of patients received both palliative radiotherapy and chemotherapy, 31.8% received palliative radiotherapy alone and 0.4% received palliative chemotherapy alone. The median OS was 13.5 months (IQR: 6.4- 19.7) and the median PFS was 5.3 months (IQR: 1.6- 12.8) in the palliative group.
Conclusion
Sinonasal tumors are a complex and diverse group of cancers. The advanced stage of presentation, histologic diversity, and anatomical proximity to critical neurovascular structures make the treatment of SNM challenging. The median OS was 35.6 months and the median PFS was 29.5 months, with inferior PFS in advanced-stage disease. Early diagnosis and multi-disciplinary approach are imperative in the management of SNM.