The Impact of Joint Radiologist Input in Head and Neck Radiotherapy Peer Review on MDT's TNM Classification and Outcome
Purpose/Objective
Accurate TNM classification and staging in head and neck cancer is an important part in prognostication, and in determining the extent of radiotherapy target volume delineation [1]. As standard of care locally, the TNM classification is performed in 2 regional supra-multidisciplinary team (MDT) meetings, prior to referral centrally for oncological treatment.
Peer review quality assurance of radiotherapy volumes is a widely accepted and recommended practice. As a tertiary cancer centre, there is routine radiologist input in the departmental peer review of head and neck radiotherapy volumes [2]. The aim of this study was to evaluate the recommended treatment changes, and potential differences between the final peer review's TNM classification and of the MDTs’.
Material/Methods
All head and neck intensity modulated radiotherapy (IMRT) cases discussed in the weekly peer review meeting between May and mid-October 2023 were prospectively evaluated. A standard data collection proforma based on UK Royal College of Radiologists (RCR) recommendations was used [3]. Any radiological/clinical progression of disease (PD) since the diagnostic radiology, final TNM staging, in addition to the RCR defined ‘major’ or ‘minor’ changes to the clinical target volumes (CTVs), were prospectively recorded.
Results
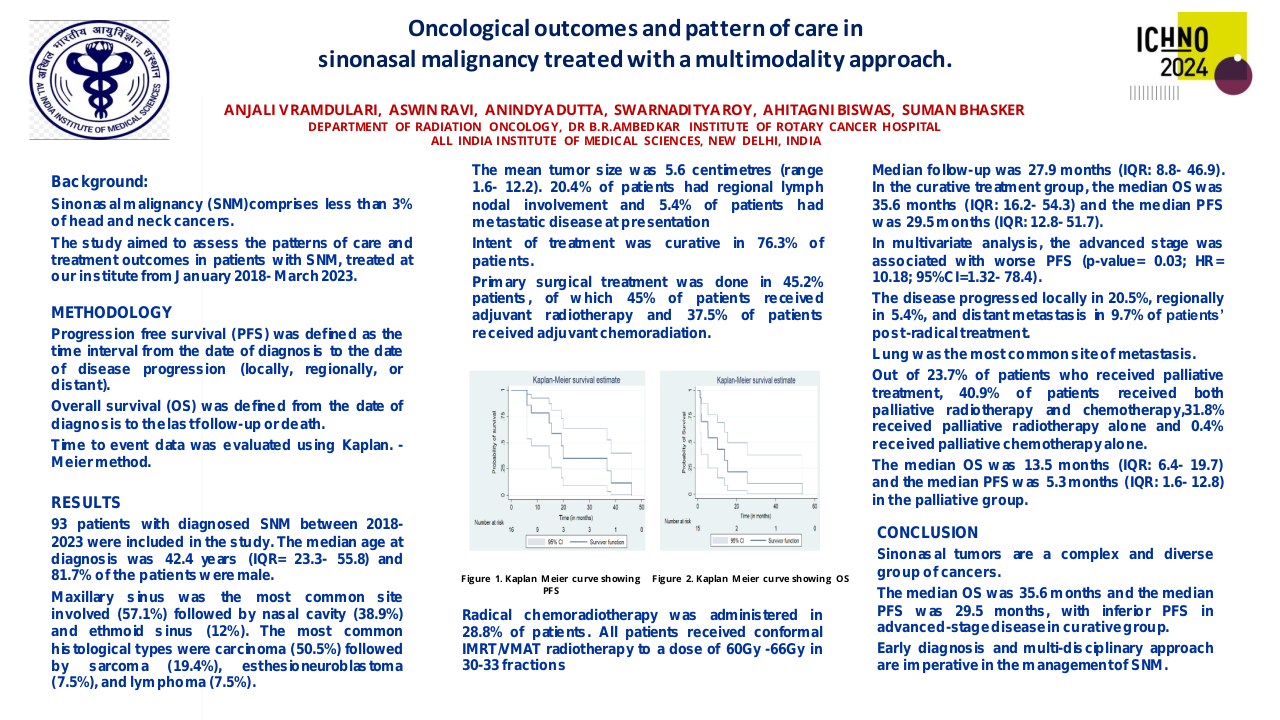
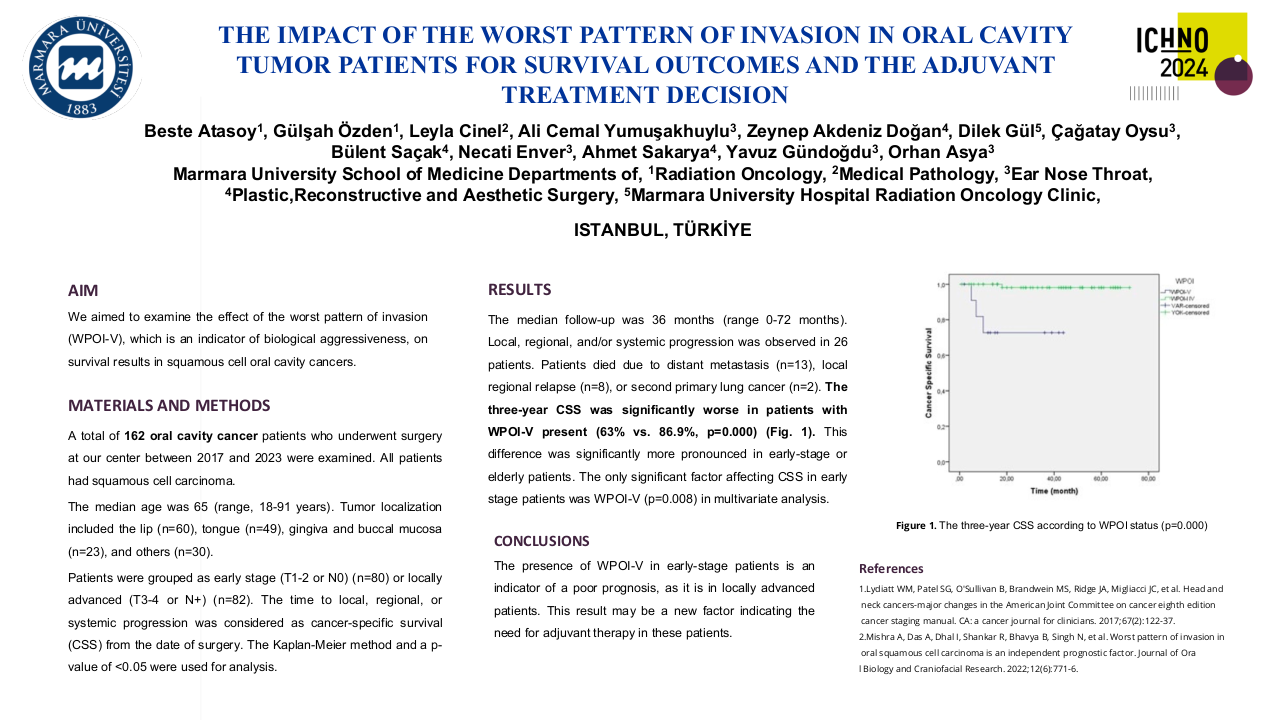
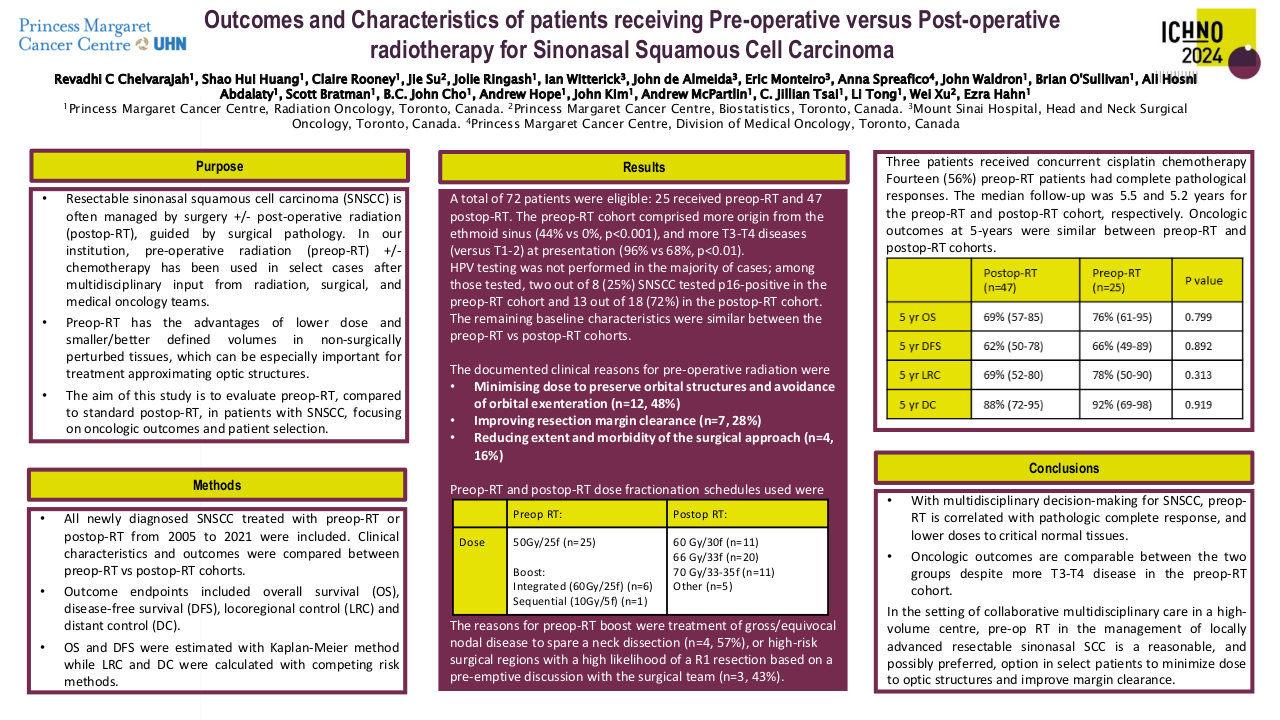
A total of 109 patients were included, of which there were 77 (71%) definitive (chemo)IMRT, 30 (28%) post-operative radiation (PORT) and 2 complex palliative IMRT (2%). Across all three cohorts, there were 34 (32%) HPV-mediated oropharynx, 21 (19%) Larynx, 18 (17%) Oral cavity, 10 (9%) Hypopharynx, 7 (6%) Nasopharynx, 6 5.5%) Cutaneous carcinoma, 4 (4%) Major salivary gland, 3 (3%) p16-negative Oropharynx, 3 (3%) Nasal cavity/Paranasal sinuses, and 3 (3%) unknown primary cases. There was a median of 2 consultant oncologists (range 1–4), and one radiologist (range 0 – 3) at each meeting.
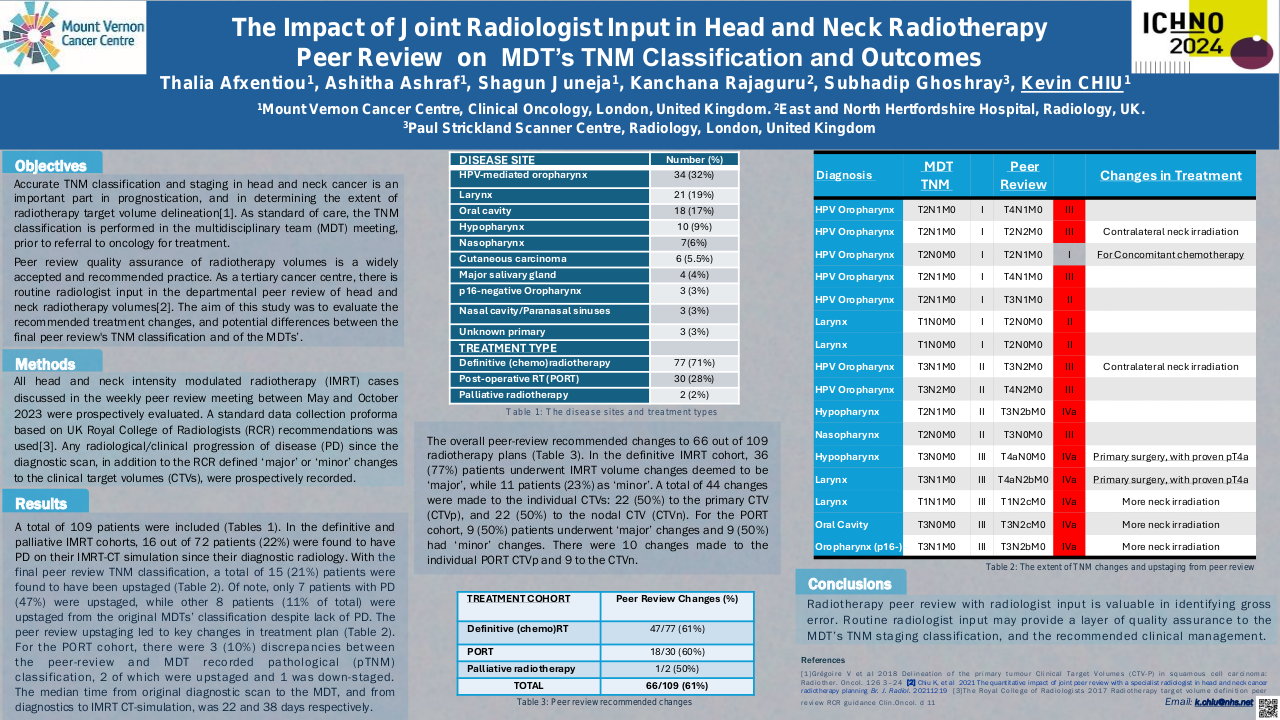
In the definitive and palliative IMRT cohorts, excluding 7 patients who had received induction chemotherapy (6 Nasopharynx, 1 Nasal cavity), 16 out of 72 patients (22%) were found to have PD on their IMRT-CT simulation since their diagnostic radiology. With the final peer review TNM classification, a total of 15 (21%) patients were found to have been upstaged (Table 1). Of note, only 7 patients with PD (47%) were upstaged, while other 8 patients (11% of total) were upstaged from the original MDTs’ classification despite lack of PD. The peer review upstaging led to 3 key changes in treatment plan, with 2 patients subsequently recommended for primary surgery instead, and 1 patient for additional concomitant chemotherapy. The median time from original diagnostic radiology to the MDT, and from diagnostics to IMRT-CT simulation, was 22 and 38 days respectively. For the PORT cohort, there were 3 (10%) discrepancies between the peer-review and the MDT recorded pathological (pTNM) classification: 2 patients were upstaged and 1 was down-staged.
| Diagnosis | MDT TNM | MDT Stage | Peer review TNM | Peer Review Stage | Treatment change |
| HPV Mediated Oropharynx | T2N1M0 | I | T4N1M0 | III | |
| HPV Mediated Oropharynx | T2N1M0 | I | T2N2M0 | III | Contralateral neck irradiation |
| HPV Mediated Oropharynx | T2N0M0 | I | T2N1M0 | I | Concomitant chemotherapy, no upstage |
| HPV Mediated Oropharynx | T2N1M0 | I | T4N1M0 | III | |
| HPV Mediated Oropharynx | T2N1M0 | I | T3N1M0 | II | |
| Larynx | T1N0M0 | I | T2N0M0 | II | |
| Larynx | T1N0M0 | I | T2N0M0 | II | |
| HPV Mediated Oropharynx | T3N1M0 | II | T3N2M0 | III | More contralateral neck irradiation |
| HPV Mediated Oropharynx | T3N2M0 | II | T4N2M0 | III | |
| Hypopharynx | T2N1M0 | II | T3N2bM0 | IVa | |
| Nasopharynx | T2N0M0 | II | T3N0M0 | III | |
| Hypopharynx | T3N0M0 | III | T4aN0M0 | IVa | Primary surgery, with proven pT4a |
| Larynx | T3N1M0 | III | T4aN2bM0 | IVa | Primary surgery, with proven pT4a |
| Larynx | T1N1M0 | III | T1N2cM0 | IVa | More neck irradiation |
| Oral Cavity | T3N0M0 | III | T3N2cM0 | IVa | More neck irradiation |
| Oropharynx (p16-) | T3N1M0 | III | T3N2bM0 | IVa | More neck irradiation |
Table 1: The extent of TNM upstage and changes
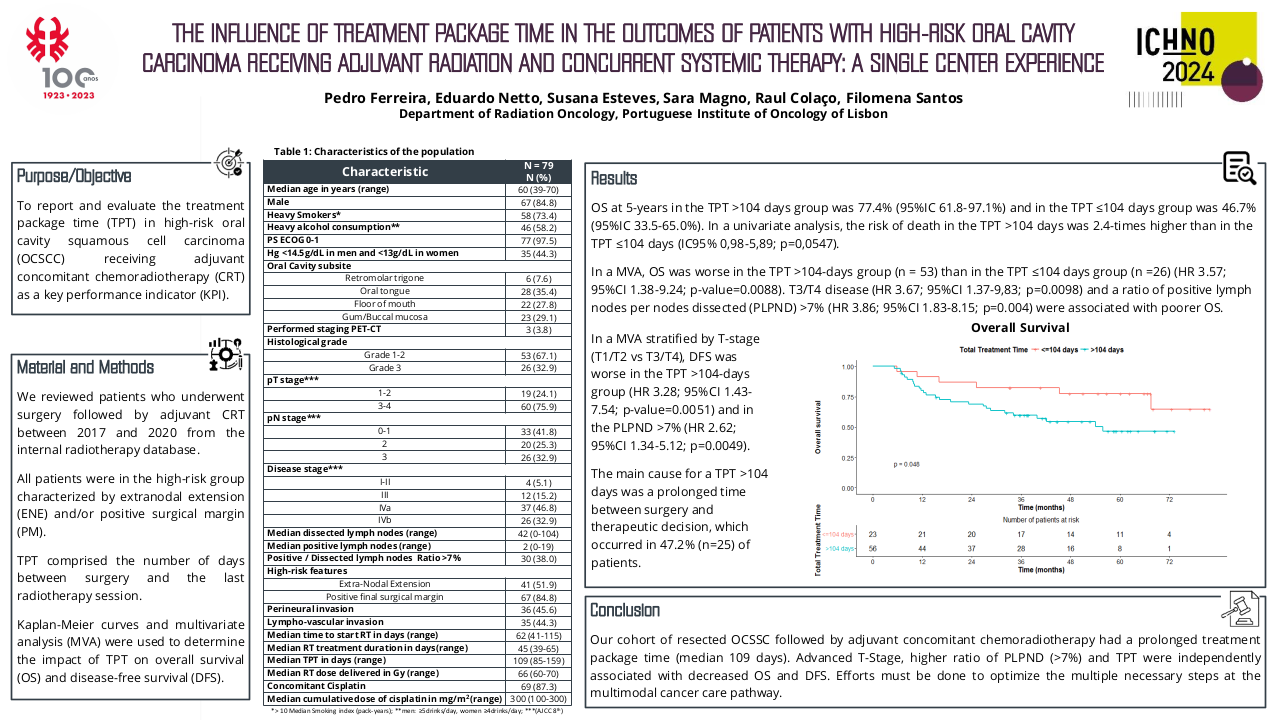
For the IMRT volume quality assurance, the peer review recommended changes to 66 out of the 109 (61%) patients; 47 out of 77 (61%) definitive IMRT, 18 out of 30 (60%) PORT, and 1 out of 2 (50%) palliative patients. In the definitive IMRT cohort, 36 (77%) patients underwent IMRT volume changes deemed to be ‘major’, while 11 patients (23%) as ‘minor’. A total of 44 changes were made to the individual CTVs: 22 (50%) to the primary CTV (CTVp), and 22 (50%) to the nodal CTV (CTVn). For the PORT cohort, 9 (50%) patients underwent ‘major’ changes and 9 (50%) had ‘minor’ changes. There were 10 changes made to the individual PORT CTVp, and 9 to the CTVn.
Conclusion
Radiotherapy peer review with radiologist input is valuable in identifying gross error. Routine radiologist input may provide an additional layer of quality assurance to the MDT’s TNM staging classification, and the subsequent recommended clinical management.
[1] Grégoire V, Evans M, Le Q T, Bourhis J, Budach V, Chen A, Eisbruch A, Feng M, Giralt J, Gupta T, Hamoir M, Helito J K, Hu C, Hunter K, Johansen J, Kaanders J, Laskar S G, Lee A, Maingon P, Mäkitie A, Micciche F, Nicolai P, O’Sullivan B, Poitevin A, Porceddu S, Składowski K, Tribius S, Waldron J, Wee J, Yao M, Yom S S, Zimmermann F and Grau C 2018 Delineation of the primary tumour Clinical Target Volumes (CTV-P) in laryngeal, hypopharyngeal, oropharyngeal and oral cavity squamous cell carcinoma: AIRO, CACA, DAHANCA, EORTC, GEORCC, GORTEC, HKNPCSG, HNCIG, IAG-KHT, LPRHHT, NCIC CTG, NCRI, NRG Oncolog Radiother. Oncol. 126 3–24[2] Chiu K, Hoskin P, Gupta A, Butt R, Terparia S, Codd L, Tsang Y, Bhudia J, Killen H, Kane C, Ghoshray S, Lemon C and Megias D 2021 The quantitative impact of joint peer review with a specialist radiologist in head and neck cancer radiotherapy planning Br. J. Radiol. 20211219[3] The Royal College of Radiologists 2017 Radiotherapy target volume definition and peer review RCR guidance Clin. Oncol. d 11