THE INFLUENCE OF TREATMENT PACKAGE TIME IN THE OUTCOMES OF PATIENTS WITH HIGH-RISK ORAL CAVITY CARCINOMA RECEIVING ADJUVANT RADIATION AND CONCURRENT SYSTEMIC THERAPY: A SINGLE CENTER EXPERIENCE
Purpose/Objective
To document and report the treatment package time (TPT) in high-risk oral cavity squamous cell carcinoma (OCSCC) receiving adjuvant treatment with concomitant chemoradiotherapy (CRT) as a quality performance indicator.
Material/Methods
We selected patients who underwent surgery followed by adjuvant CRT between 2017 and 2020 from the internal radiotherapy database. All patients were in the high-risk group characterized by extranodal extension (ENE) and/or positive surgical margin (PM). TPT comprised the number of days between surgery and the last radiotherapy session. Kaplan-Meier curves and multivariate analysis (MVA) were used to determine the impact of TPT on overall survival (OS) and disease-free survival (DFS).
Results
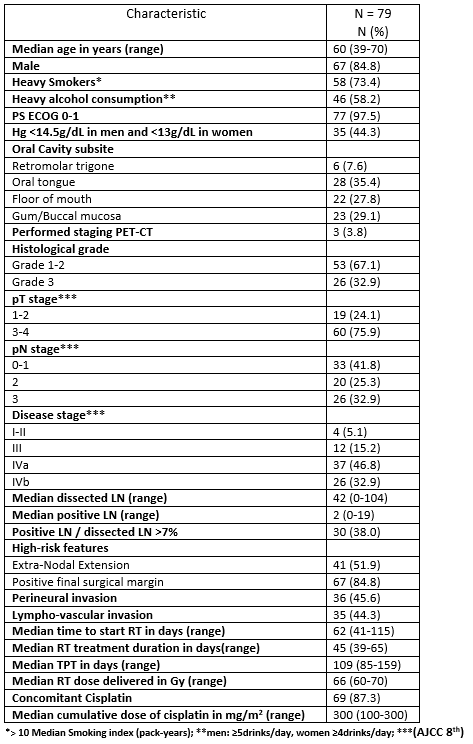
A total of 79 patients were included with a median age of 60 years (range: 39–70 years), a majority of male patients (84.8%, n=67) and heavy smokers (73.4%, n=58). The most frequent primary tumor locations were oral tongue (35.4%, n=28), gum/buccal mucosa (29.1%, n=23) and floor of the mouth (27.8%, n=22). ENE and PM were detected in 51.9% (n=41) and 84.8% (n=67) of cases, respectively. Median radiotherapy dose was 66Gy. Median cisplatin concomitant dose was 300mg/m2. Median TPT was 109 days (85–159).
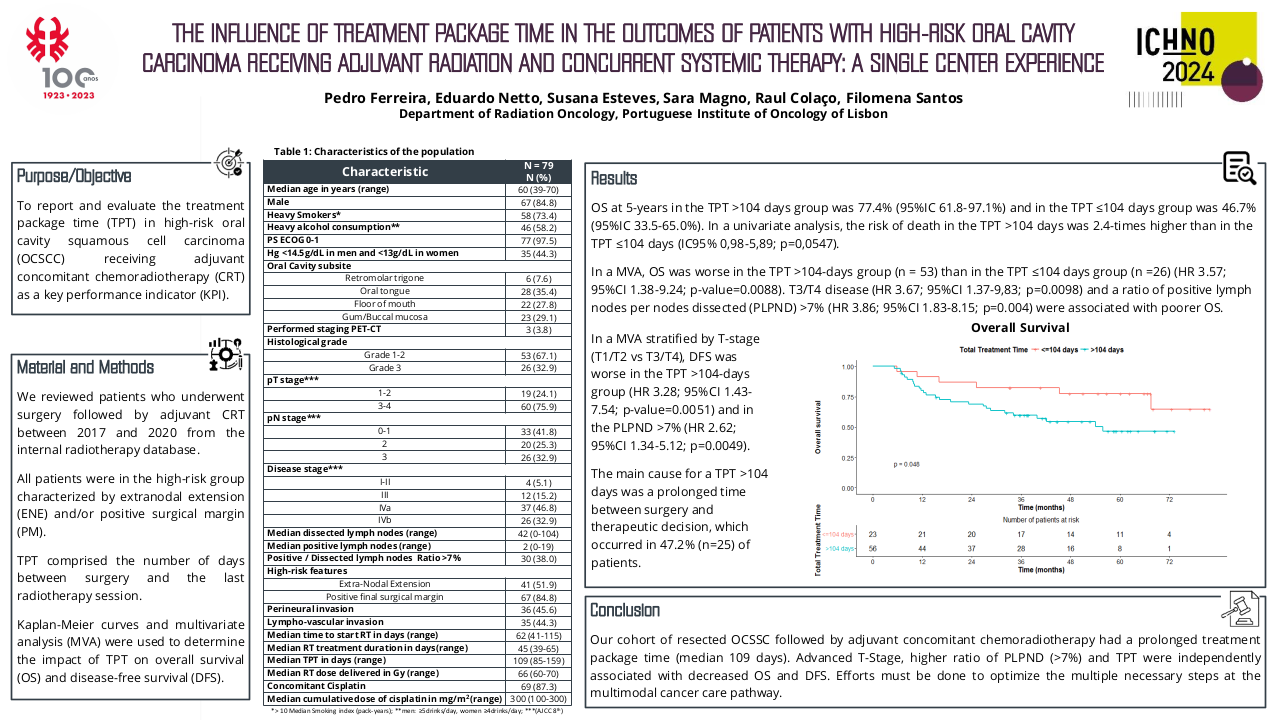
Table 1 – Population characteristics of the study cohort
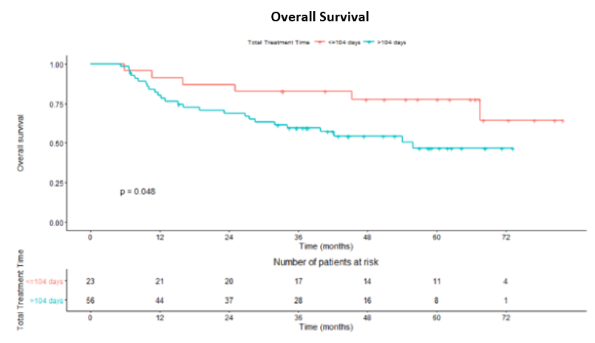
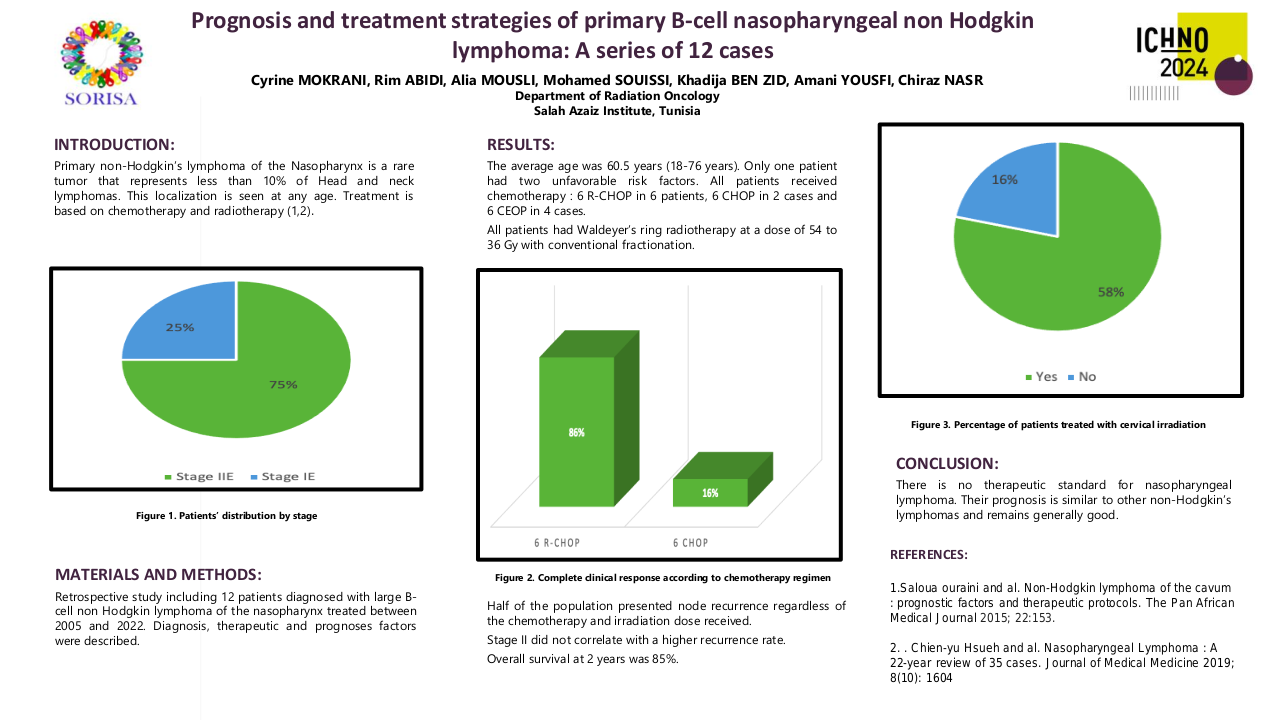
OS at 5-years in the TPT >104 days group was 77.4% (95%IC 61.8-97.1%) and in the TPT ≤104 days group was 46.7% (95%IC 33.5-65.0%). In a univariate analysis, the risk of death in the TPT >104 days was 2.4-times higher than in the TPT ≤104 days (IC95% 0,98-5,89; p=0,0547). In a MVA, OS was worse in the TPT >104-days group (n = 53) than in the TPT ≤104 days group (n =26) (HR 3.57; 95%CI 1.38-9.24; p-value=0.0088). T3/T4 disease (HR 3.67; 95%CI 1.37-9.83; p=0.0098) and a ratio of positive lymph nodes per nodes dissected (PLPND) >7% (HR 3.86; 95%CI 1.83-8.15; p=0.004) were associated with poorer OS. In a MVA stratified by T-stage (T1/T2 vs T3/T4), DFS was worse in the TPT >104-days group (HR 3.28; 95%CI 1.43-7.54; p-value=0.0051) and in the PLPND >7% (HR 2.62; 95%CI 1.34-5.12; p=0.0049). The main cause for a TPT >104 days was a delay in therapeutic decision, which occurred in 47.2% (n=25) of patients.
Conclusion
Our cohort of resected OCSSC followed by adjuvant concomitant chemoradiotherapy had a prolonged treatment package time (median 109 days). Advanced T-Stage, higher ratio of PLPND (>7%) and TPT were independently associated with decreased OS and DFS. Efforts must be done to optimize the multimodal cancer care pathway.