Reirradiation with Stereotactic Ablative Radiotherapy in Recurrent Nasopharyngeal Carcinoma
Purpose/Objective
Local recurrence (LR) rates in nasopharyngeal carcinoma (NPC) following definitive radiation (RT) ± chemotherapy (CT) range from 7–15%. A prospective trial comparing endoscopic surgery and re-irradiation in recurrent cases found that surgery improved survival in a carefully chosen group of patients with low-volume mucosal recurrence. However, the fact that the recurrent disease is mostly multifocal and infiltrative in nature makes a limited group of patients suitable for surgery. In this study, we aimed to report our stereotactic ablative radiotherapy (SABR) outcomes in cases diagnosed with recurrent NPC.
Material/Methods
The data of 83 patients who underwent SABR in our department between 2007 and 2022 with the diagnosis of local-regional recurrent NPC, which was unresectable or had surgical margin positivity after resection were evaluated retrospectively. The Kaplan-Meier method was used for survival analyses (IBM SPSS v.23).
Results
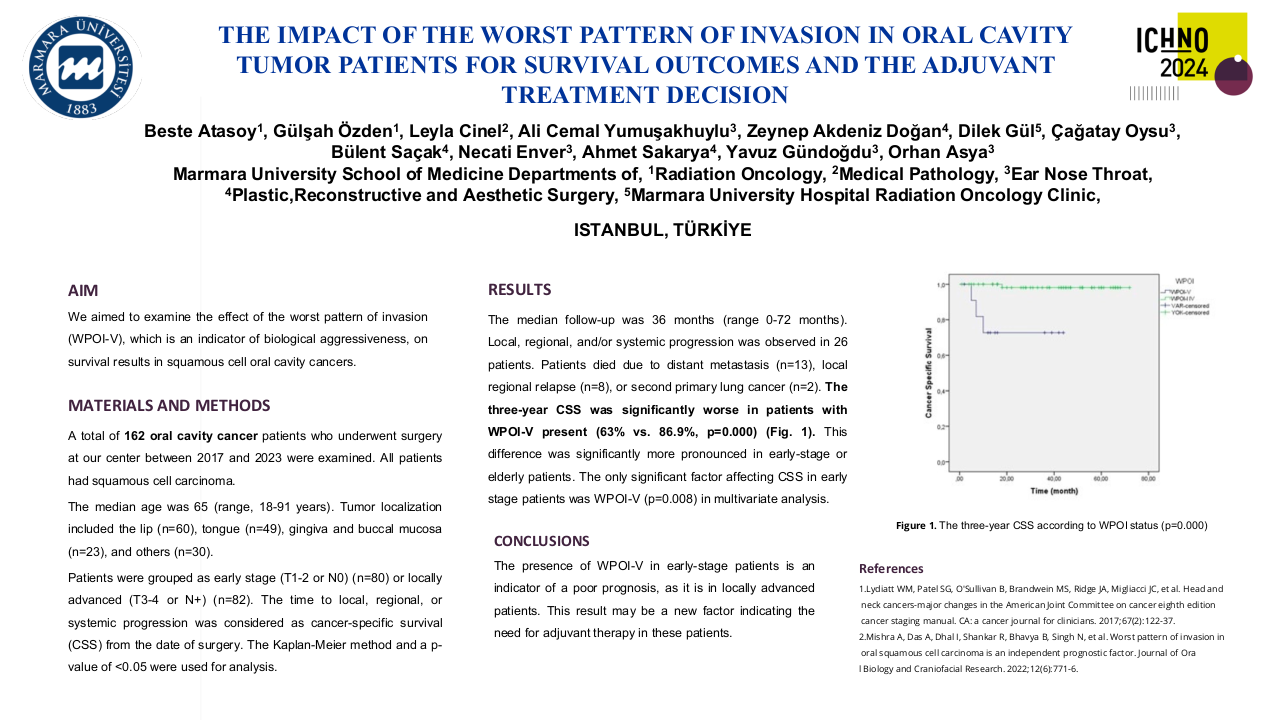
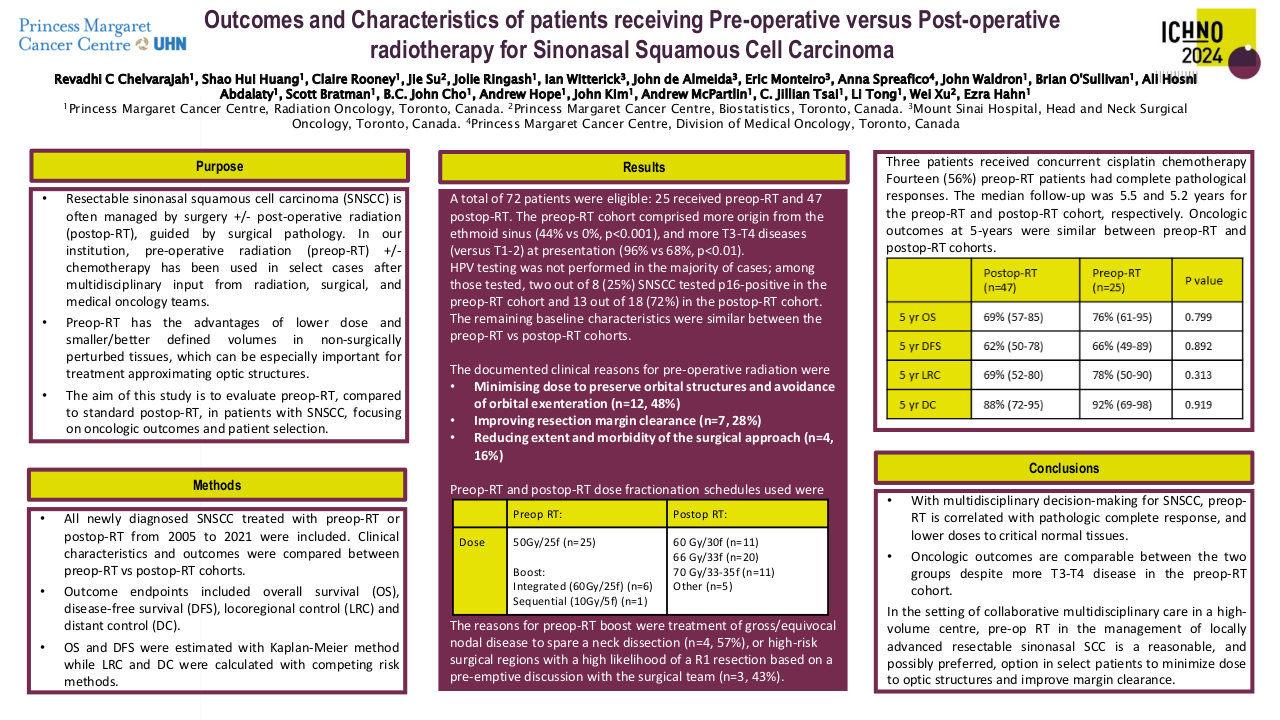
Patient, tumor, and treatment characteristics are presented in Table 1. The median age was 53 (range, 19-78). The median follow-up was 24 months (range, 3–151 months). The median interval between patients' first and second RT's was 39 months (range, 4–238 months). The initial response evaluation following reirradiation found a complete response in 38%, a partial response in 40%, stable disease in 8%, and progression in 1%. In follow-up, LR developed in 20 patients (24%) and distant metastasis (DM) developed in 14 patients (17%). The most common sites of DM were the lung, bone, and liver. SABR provided 76% local control (LC). The 1- and 2-year overall survival (OS), local recurrence-free survival (LRFS), and distant metastasis-free survival (DMFS) rates were 67% and 53%, 65% and 46%, and 62% and 49%, respectively. In univariate analysis, LRFS (60% vs. 34%, p=0.002) and DMFS (63% vs. 31%, p=0.007) rates were higher in patients with recurrent tumor volume ≤36 cc compared to patients with tumor volume >36 cc. Age (≤53 vs. >53 years), gender (male vs. female), interval between RTs (≤2 vs. >2 years), surgery before SBRT (yes vs. no), SBRT dose (≤30 vs. >30 Gy) and device (robotic- vs. linear accelerator-based), and site of recurrence (primary vs. neck recurrence) could not be identified for prognostic significance for OS, LRFS, and DMFS parameters. A notable proportion of patients experienced late toxicity, with 20% exhibiting grade 3 or 4 toxicity and 12% experiencing grade 5 toxicity. Fourteen patients (17%) experienced massive hemorrhage as a result of carotid blow-out syndrome (CBOS); two patients (2%) suffered from cerebrovascular disease as a result of carotid artery stenosis; five patients (6%) experienced brain parenchymal necrosis; three patients (3.5%) had permanent gastrostomies; and three patients (3.5%) had hearing loss. There was no observed disparity in toxicity levels between doses administered consecutively or every other day.
Table 1. Patient, tumor, and treatment characteristics.
| Characteristic |
Number of Patients (n=83, %) |
|
Gender Male Female |
56 (67.5) 27 (32.5) |
|
Interval between RT’s (median) <2 year ≥2 year |
39 months (4-238 months) 29 (35) 54 (65) |
| RT dose, median (range) / fractions, median (range) |
70 Gy (60-74 Gy) / 33 fractions (30-33) |
|
Recurrence location Primary Neck Primary and neck |
73 (88) 4 (5) 6 (7) |
| SABR dose / fractions (median) |
30 Gy (24-50 Gy) / 5 (1-6) |
|
SABR technique CyberKnife© Novalis® Linac (VMAT) |
72 (87) 8 (9) 3 (4) |
|
Fractionation Consecutive days Every other day |
63 (76) 20 (24) |
| GTV volume, median (range) |
36 cc (1-204 cc) |
|
Treatment outcomes Complete response Partial response Stabile disease Progression Unknown |
31 (38) 33 (40) 6 (8) 1 (1) 11 (13) |
Conclusion
Using SABR as a reirradiation method for people with recurrent NPC has shown to be very effective at achieving LC while keeping treatment-related side effects at a level that can be tolerated. There is a positive correlation between a smaller recurring tumor volume and higher levels of local recurrence-free survival (LRFS) and distant metastasis-free survival (DMFS).