Time from surgery to commencing adjuvant radiotherapy does not affect survival in patients with head and neck squamous cell carcinoma
Purpose/Objective
Studies have reported inferior outcomes when adjuvant radiotherapy starts more than 6-8 weeks post-surgery for locally-advanced head and neck squamous cell carcinoma (HNSCC). However, the applicability of these studies may be limited due to the dichotomisation of time variables (e.g.,‘on time’ vs ‘delayed’ radiotherapy) either arbitrarily or based on the sample median1-3. In clinical practice, oncologists may omit radiotherapy when delays extend beyond this time and instead advocate for observational approaches only.
This study aimed to assess the relationship between survival and the time interval between surgery and radiotherapy as a continuous variable. We hypothesised there would be no significant change in survival around either six or eight weeks post-surgery.
Material/Methods
An institutionally approved, retrospective review of prospectively collected data. Inclusion criteria: all patients with HNSCC who underwent curative-intent surgery followed by post-operative (chemo)radiotherapy at The Christie NHS Foundation Trust (UK) between Jan 2014 and Dec 2020. Patient, cancer and treatment data were collected. Time intervals of interest included (i) days from surgery to radiotherapy start and (ii) overall treatment time (OTT; days from surgery to radiotherapy completion).
Demographic and cancer details were summarised using descriptive statistics. A multiple linear regression model was fitted to assess associations between patient / tumour characteristics and time from surgery to radiotherapy. The primary endpoint was overall survival (OS). A multivariable Cox Proportional Hazards (PH) model was fitted. Missing values were handled by multiple imputation using chained equations.
Results
386 patients were included. Patient characteristics are shown in the Table.
| Characteristic | N = 3861 |
| Age (median, IQR) | 65 (56-71) |
| Gender | |
| Female | 120 (31%) |
| Male | 266 (69%) |
| ECOG performance status | |
| 0 | 94 (24%) |
| 1 | 193 (50%) |
| 2 | 79 (21%) |
| 3 | 19 (4.9%) |
| ACE-27 score | |
| 0 | 166 (43%) |
| 1 | 133 (35%) |
| 2 | 64 (17%) |
| 3 | 21 (5.5%) |
| Smoking history | |
| Current | 70 (19%) |
| Ex | 214 (59%) |
| Never | 80 (22%) |
| H&N subsite | |
| Larynx | 45 (12%) |
| Oral cavity | 214 (55%) |
| Pharynx | 103 (27%) |
| Nose / sinuses | 24 (6.2%) |
| Surgical margin status | |
| <1mm | 164 (44%) |
| 1-5mm | 149 (40%) |
| >5mm | 59 (16%) |
| Tumour stage | |
| T1 | 53 (14%) |
| T2 | 111 (24%) |
| T3 | 57 (15%) |
| T4 | 157 (42%) |
| Nodal stage | |
| N0 | 130 (34%) |
| N1 | 77 (20%) |
| N2 | 44 (11%) |
| N3 | 135 (35%) |
| Treatment modality | |
| Chemo-RT | 110 (28%) |
| RT alone | 276 (72%) |
| Radiotherapy schedule | |
| 4 weeks | 75 (19%) |
| 6 weeks | 310 (81%) |
The median time between surgery and radiotherapy start was 44 days (IQR: 14 days). 175 patients (45.3%) commenced radiotherapy within six weeks of surgery, and 317 (82.1%) within eight weeks. The median OTT was 83 days (IQR: 14 days).
On multivariable linear regression, the time interval between surgery and radiotherapy start was not associated with any candidate covariate (as listed in Table). The multiple R-squared value for the model was 0.07 (i.e., the model accounted for only 7% of variability in the time between surgery and radiotherapy start).
There were 154 OS events at a median of 1.65 years (IQR 2.46 years) For surviving patients (n = 232), the median follow-up was 4.57 years (IQR 2.59 years).
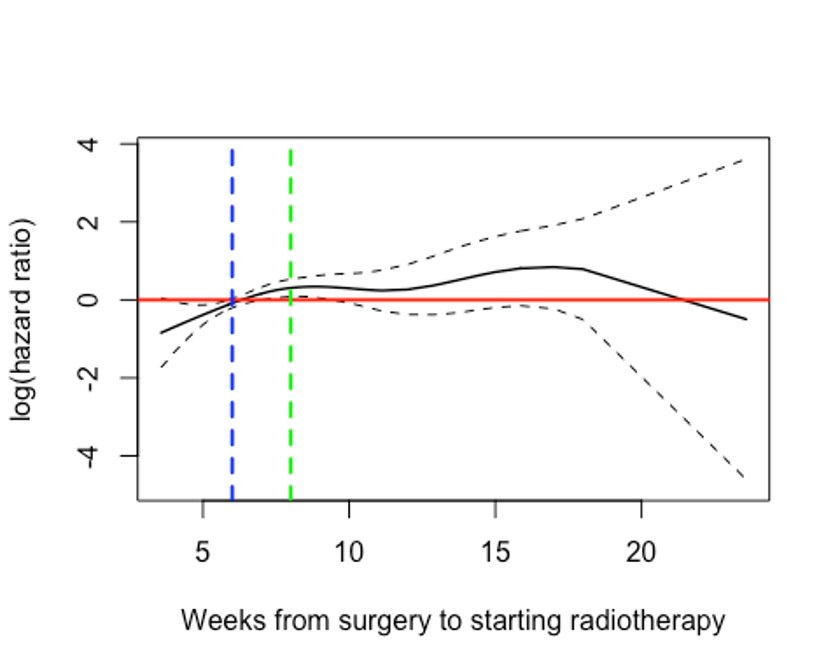
To explore the relationship between OS and days from surgery to starting radiotherapy, the two variables were plotted (Figure). While log(hazard) for OS increased around 6 weeks post-surgery, the increase was small before falling again at 8 weeks post-surgery. The risk only increased again at ~ 12 weeks post-surgery, although inferences become difficult at this point due to small patient numbers.
On multivariable Cox regression, the time interval between surgery and radiotherapy start was not associated with OS (HR 1.00; 95% CI 0.99 - 1.01; p=0.5). A further Cox model was fitted, with OTT as an alternative covariate; this too was not prognostic (HR 1.01; 95% CI 0.94 - 1.09; p=0.7).
Conclusion
In this study, neither an increasing time interval between surgical resection and commencing post-operative radiotherapy nor increasing OTT was associated with inferior OS for patients with resected HNSCC, when adjusted for demographic, clinical and treatment-related covariables. We recommend that patients are still considered for adjuvant radiotherapy even in the presence of a delay post-surgery of > 6-8 weeks.
1. Vikram, B. Importance of the time interval between surgery postoperative radiation therapy in the combined management of head & neck cancer. International Journal of Radiation Oncology*Biology*Physics 5, 1837–1840 (1979).2. Rosenthal, D. I. et al. Importance of the treatment package time in surgery and postoperative radiation therapy for squamous carcinoma of the head and neck. Head Neck 24, 115–126 (2002).3. Tribius, S. et al. Survival and overall treatment time after postoperative radio(chemo)therapy in patients with head and neck cancer: Overall treatment time and survival after postoperative radio(chemo)therapy in head and neck cancer. Head Neck 38, 1058–1065 (2016).